- Center on Health Equity and Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Disease-, Age-, Genomic-Specific Factors Increase Risk of ET, PV, PrePMF Developing Into Overt MF
New research highlights the factors that increase the likelihood that essential thrombocytopenia (ET), polycythemia vera (PV), and prefibrotic primary myelofibrosis (PrePMF) will evolve into overt myelofibrosis (MF).
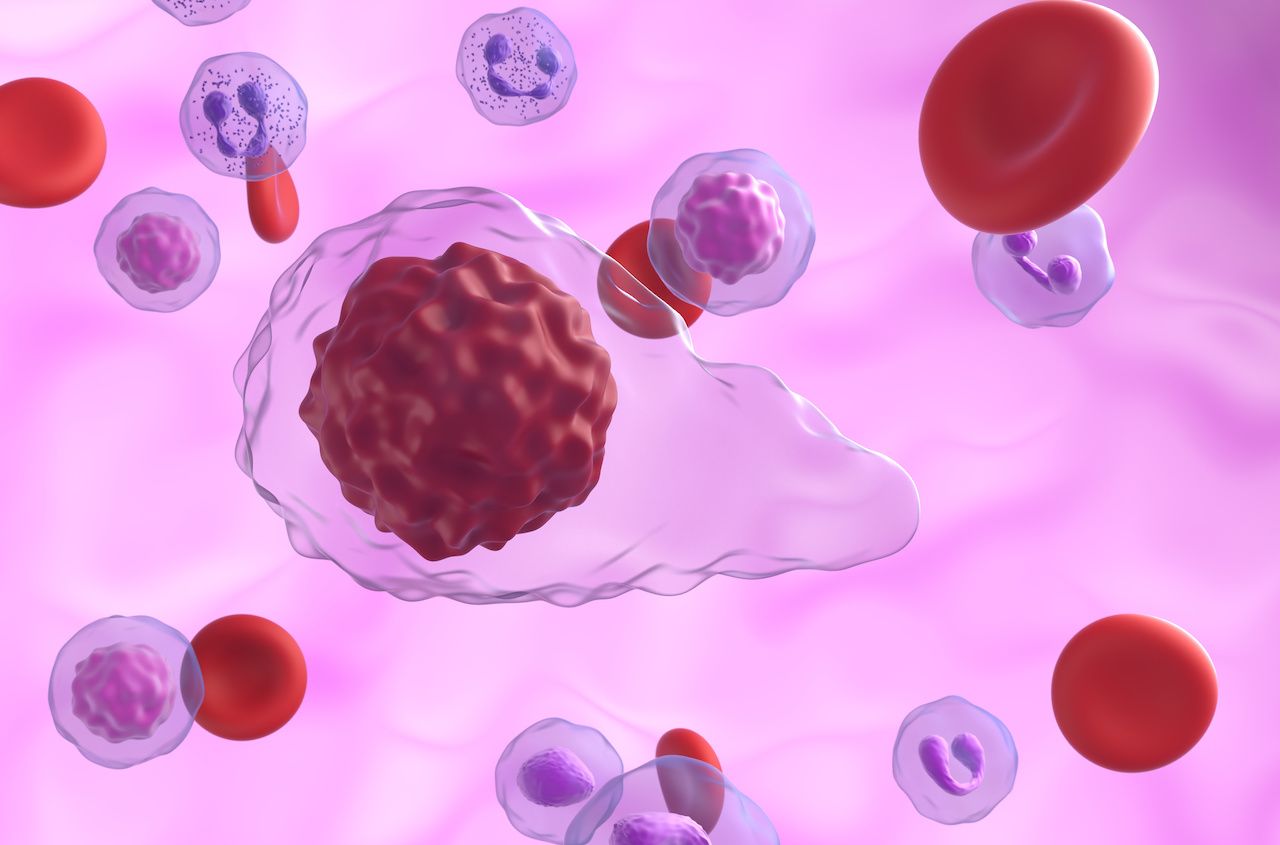
Primary myelofibrosis cells | Image credit: LASZLO - stock.adobe.com
The risk of essential thrombocytopenia (ET), polycythemia vera (PV), and prefibrotic primary myelofibrosis (PrePMF) developing into overt myelofibrosis (MF) increases with age, the accumulation of mutations, and the activation of proliferative pathways, which identifies new targets for therapeutic intervention.
The findings, based on an analysis of the mutational landscape of more than 1700 genes and the gene expression of various cells from patients with myeloproliferative neoplasms (MPNs), was published in Clinical Cancer Research.1
ET, PV, PMF, and MF are all part of a group of diseases MPNs, in which a mutation in the bone marrow causes too many red blood cells, white blood cells, or platelets.2 In addition to being the most common MPNs, ET, PV, and PMF share the presence of mutations in either Janus kinase 2 (JAK2), calreticulin (CALR), and/or MPL.3 ET and PV are less aggressive forms of MPN, but they still can progress to MF. According to the Leukemia & Lymphoma Society, Pre-PMF will likely progress to PMF, “suggesting that more regular observations for pre-fibrotic PMF patients is warranted.”3
“Based on clinical presentation, MF clearly represents a progression of ET/PV/PrePMF; nevertheless, molecular mutations and transcriptional and epigenetic events associated with this phenotypic transition are not well defined,” the authors explained.1
Patients with malignancies enrolled in the Mi-ONCOSEQ study were included in this sequencing study. There were 216 patients with suspected ET, PV, PrePMF, or MF included who had peripheral blood (PB) or bone marrow (BM) samples collected. Of these patients, 163 received a confirmed diagnosis of ET, PV, PrePMF, or MF. After next-generation sequencing (NGS) testing, there were 139 samples with adequate tumor content: 108 patients with MF and 31 with ET/PV/PrePMF.
In both cohorts, 45% of the patients were female. The median age of the MF was higher at 68 years compared with 63 years for the ET/PV/PrePMF cohort. Patients with MF had lower hemoglobin levels, a higher leukocyte count, and a higher percentage of abnormal karyotypes. While both cohorts had JAK2, CALR, and MPL mutations, only the MF cohort had 2 patients with both JAK2 and MPL mutations, plus there were 4 patients with no driver gene mutations.
The researchers also sequences a panel of 1711 genes:
- 490 somatic variants were identified in the 237 genes from the MF cohort
- 146 somatic variants were identified in the 77 genes for the ET/PV/PrePMF cohort
- The MF cohort had a higher burden of somatic mutations with an average of 5.5 mutations per case vs 4.3 per case
- Patients with ET had the lowest burden (3.1/case), followed by PV (4.6/case), and PrePMF (4.7/case)
- Only 22 (7.5%) of the genes were mutated in both cohorts
In the MF cohort, there was a direct correlation of number of somatic mutations as a function of age; however, there was no correlation for the ET/PV/PrePMF cohort. Also, the more variants in patients with MF, the worse their overall survival.
“Understanding the disease transformation to MF has highlighted many factors 1) new mutations and accumulating mutations which may be a result of an unstable genome 2) epigenetic regulation, such as chromatin remodeling, which can lead to reprogramming of the hematopoietic system, 3) aberrant pathway activation such as RAS signaling which can contribute to proliferative phenotype and further disease transformation and finally 4) inflammation, cytokine secretion and transformation of medullary and extra-medullary stroma to nourish the neoplastic clone,” the authors concluded.
References
1. Kandarpa M, Robinson D, Wu Y-M, et al. Broad next generation integrated sequencing of myelofibrosis identifies disease-specific and age-related genomic alterations. Clin Cancer Res. Published online February 22, 2024. doi:10.1158/1078-0432.CCR-23-0372
2. Chronic myeloproliferative neoplasms Treatment (PDQ)—patient version. National Cancer Institute. Updated November 17, 2023. Accessed March 15, 2024. https://www.cancer.gov/types/myeloproliferative/patient/chronic-treatment-pdq
3. Myeloproliferative neoplasms (MPN) research funded by LLS. Leukemia & Lymphoma Society. Accessed March 15, 2024. https://www.lls.org/research/myeloproliferative-neoplasms-mpn-research-funded-lls
