- Center on Health Equity and Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
New Definition of Rectal Cancer Could Reduce Variability in Treatment
A new definition of rectal cancer in the Netherlands prompted reclassification of cancer as sigmoid tumors, which could lead to better treatment.
More tailored treatment of cancer could be achieved through the updated definition of rectal cancer implemented in the Netherlands, according to a study published in Colorectal Disease.1 The definition of rectal cancer was updated to the rule that rectal tumor’s lower border is located below the sigmoid take-off (STO).
Rectal and sigmoidal tumors have been hard to differentiate in the past, with guidelines often being arbitrary and the tumor definitions being combined into “rectosigmoid” tumors rather than separating them. This extend to the United States, where the boundary between sigmoid and rectal cancer still varies from study to study.2 The STO was determined to be the landmark for defining where the rectum ends and the sigmoidal tumors begin by experts of the colorectal region. However, some believe that rectal cancer diagnoses will be reduced due to the STO definition. This study aimed to retrospectively determine what the implementation of STO will do to diagnoses of rectal and sigmoid cancer and how it would affect interhospital variability.
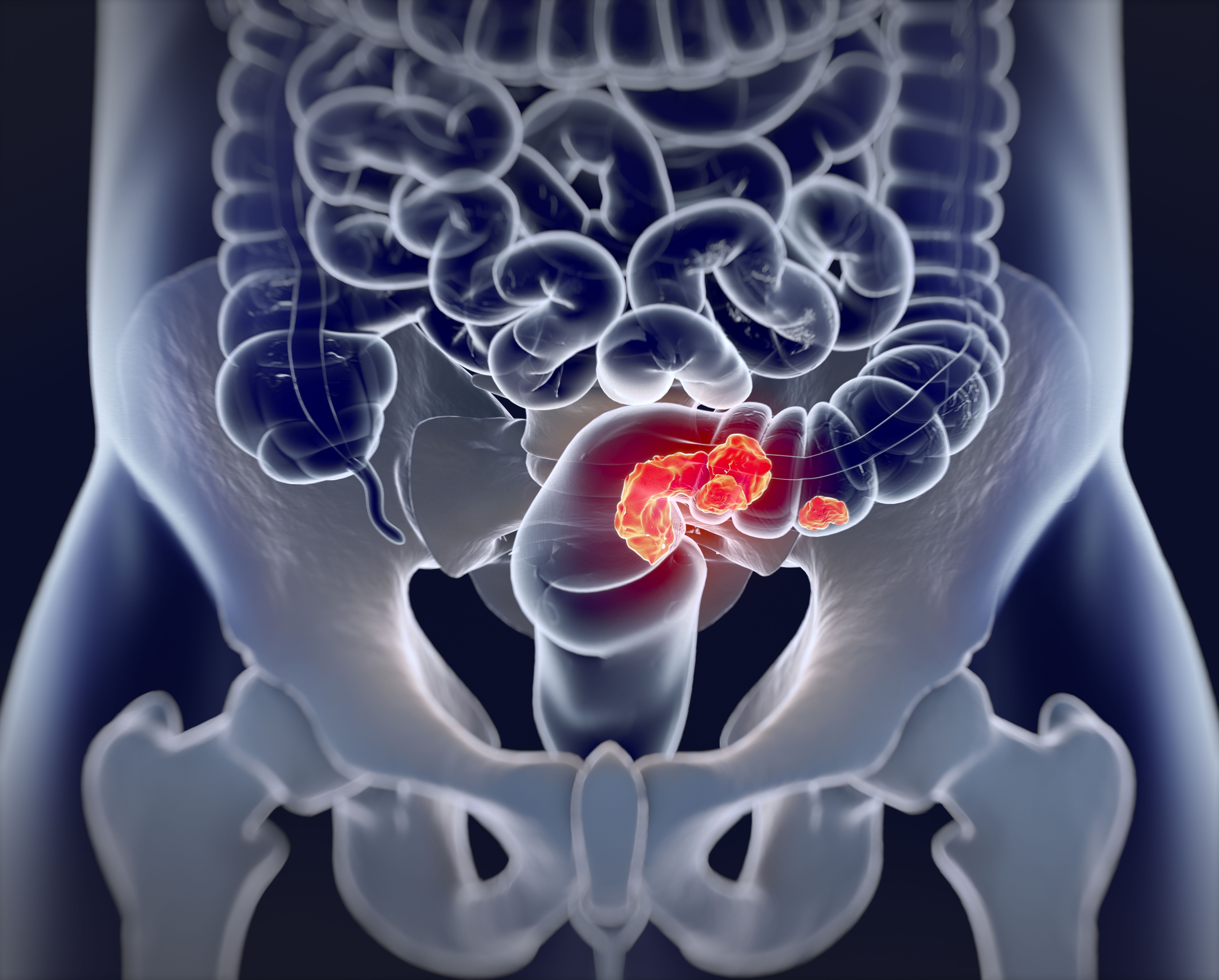
Colorectal cancer | Image credit: Anatomy Insider - stock.adobe.com
The Dutch ColoRectal Audit (DCRA) was used for this study, which contains all patients who received a surgical resection since 2009. All hospitals who had performed surgery for rectal cancer in 2016 were invited to participate in the study. Participants were included if they had rectal cancer and had a resection in 2016. Patients were excluded if they had no MRI or no visible tumor on the MRI.
These patients were included in the DCRA as having rectal cancer but the national guidelines of the time lacked a specific definition for what constituted as the rectum. Tumors were determined to be either on, above, or below the STO by evaluating MRI scans for all patients. The number of tumors reclassified as sigmoid tumors under the STO acted as the primary end point of the study. Other end points included interhospital variability and changes in treatment strategies.
There were 2784 patients across 66 hospitals who were included in this study who had a mean (SD) age of 67 (10) years and who were primarily male (65%). A total of 11% of patients were reclassified as having sigmoid cancer rather than rectal cancer when using the updated guidelines of the lower border being on the level of STO. No significant differences in demographic characteristics were found between the groups that were reclassified and weren’t reclassified. The median (IQR) proportion of tumors above the STO was 6% (1%-12%) in academic hospitals and non-academic hospitals had a median of 10% (7%-17%).
A total of 50% of the patients with a tumor above the STO were given neoadjuvant chemoradiotherapy compared with 61% who had a tumor on or below the STO. A total of 98% of patients with a tumor above the STO and 93% of patients with a tumor on or below the STO had a resection margin of more than 1.0 mm.
In a median follow up of 49 months (35.0-55.0) locoregional recurrence (LR) rate was 4% in tumors above the STO and 9% for those on or below it. Disease-free survival rate was 74% in tumors above the STO and 70% in those below the STO. Overall survival was 86% and 80% respectively. Decreased risk of LR (HR, 0.529; 95% CI, 0.298-0.939) and higher overall survival (HR, 0.732; 95% CI, 0.546-0.982) were significantly associated with patients who had a tumor above the STO.
There were some limitations to this study. The study had a retrospective nature, which could have led to the exclusion of patients who had an endoscopy to determine the type of tumor, which could lead to underreporting of sigmoid tumors. Patients could have had a diagnosis of sigmoid cancer that was changed to rectal cancer with the new STO.
The researchers concluded that these new guidelines could change the diagnosis of rectal cancer to sigmoid cancer more frequently in the future with a new STO landmark. The effect on therapy offered to each patient could be important for the treatment of rectal and sigmoid cancer in the future.
References
- Hazen SMJA, Sluckin TC, Horsthuis K, et al. Impact of the new rectal cancer definition on multimodality treatment and interhospital variability: results from a nationwide cross-sectional study. Colorectal Dis. Published online April 29, 2024. doi:10.1111/codi.17002
- Hui C, Baclay R, Liu K, et al. Rectosigmoid cancer—rectal cancer or sigmoid cancer? Am J Clin Oncol. 2022;45(8):333-337. doi:10.1097/COC.0000000000000931
Frameworks for Advancing Health Equity: Urban Health Outreach
May 9th 2024In the series debut episode of "Frameworks for Advancing Health Equity," Mary Sligh, CRNP, and Chelsea Chappars, of Allegheny Health Network, explain how the Urban Health Outreach program aims to improve health equity for individuals experiencing homelessness.
Listen
