- Center on Health Equity and Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
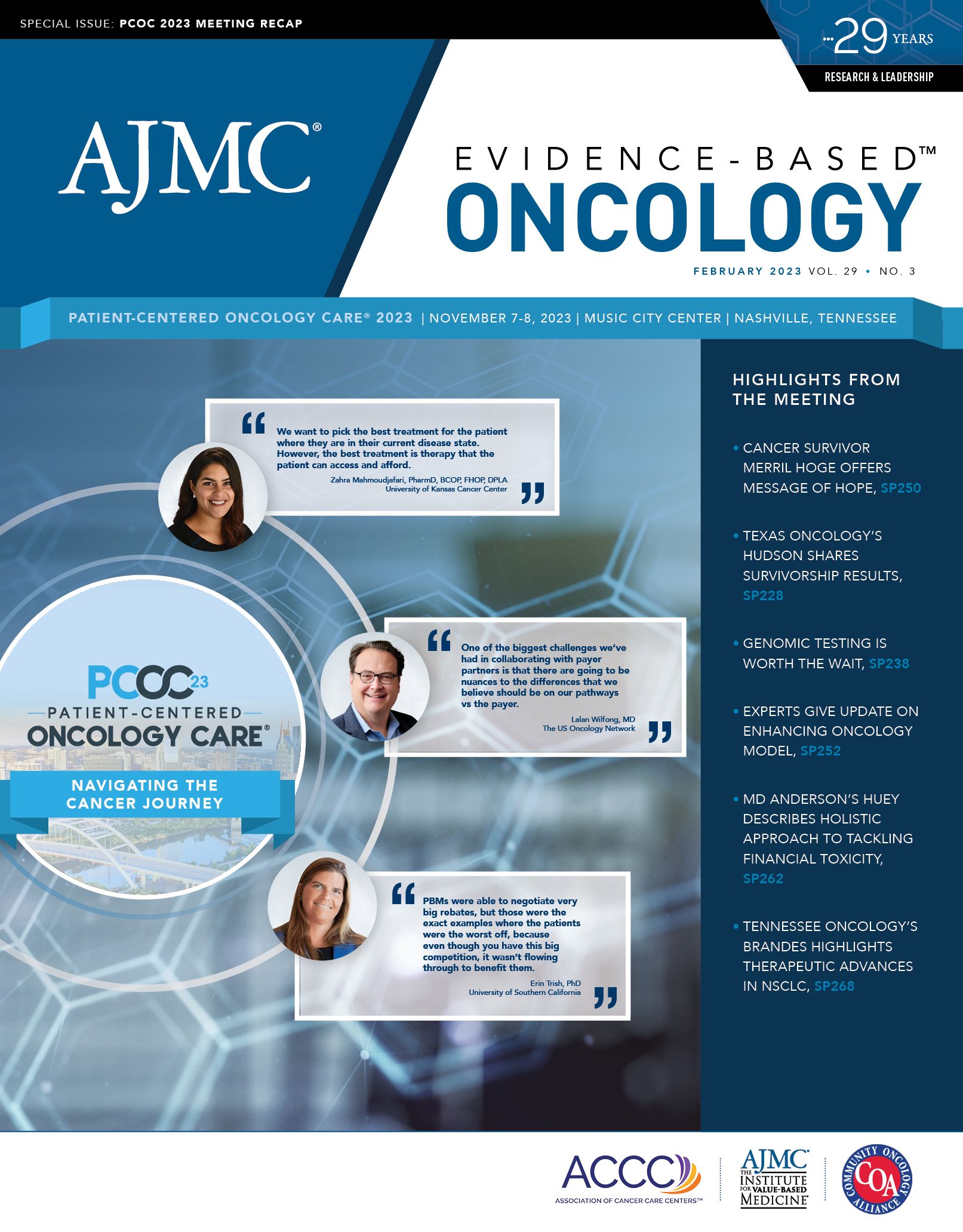
Tennessee Oncology’s Brandes Sees Progress in Biomarker Use in NSCLC, but “There’s Work to Be Done”
Coverage of Tennessee Oncology's Johann Brandes, MD, on "Precision Medicine in NSCLC."
Medical oncologist Johann Brandes, MD, can recall a time before “precision medicine” was an everyday term, when the idea of tailoring treatment to a patient’s genomic profile existed only in theory. Twenty years ago, when the FDA approved the first such treatments in non–small cell lung cancer (NSCLC), starting with the EGFR inhibitor gefitinib, “it was not called precision medicine—it was called ‘targeted therapies,’ ” he recalled.1
Johann Brandes, MD | Image: Tennessee Oncology

Ahead of his talk “Precision Medicine in NSCLC,” which he presented at Patient-Centered Oncology Care 2023 in November, Brandes, an oncologist at Tennessee Oncology in Nashville, reflected on how far the field has advanced in recent years. However, he said, “there’s still a lot of work to be done.”
The arrival of targeted therapies, Brandes noted, did not signal personalized approaches; in fact, it took clinical trials to figure out that gefitinib (Iressa) worked best in patients who were Asian and nonsmokers.1
“There are still a lot of challenges in meeting the goals of precision medicine,” he said. “We’ve gone away from a one-size-fits-all approach in cancer care, generally, and lung cancer care, specifically. But this is still the new frontier.”
As noted by other speakers during PCOC, Brandes said not enough patients are tested for mutations so that a therapeutic match can be found. When testing happens, Black patients have less access than White patients, creating inequities in care. With 15 driver mutations now identified, opportunities for personalized treatment have multiplied, he said.
Driver mutations, Brandes explained, behave like a switch for “a gene in the pulmonary and bronchial epithelium [that] is sufficient to make a cell become cancerous to make the growth go into overdrive and ultimately lead to cancer.”
By contrast, he said, turning the switch off “usually results in a very, very high likelihood for very remarkable responses.”
Why Testing Matters
A decade after the FDA approved the first targeted therapies for patients with lung cancer, the stark difference in outcomes was clear. Brandes presented data from 2014 that showed patients with NSCLC in which a driver mutation was targeted had a median survival of 3.5 years, compared with 2.4 years for those patients with driver mutations who did not receive targeted therapy.2
The benefits of genomic testing are spelled out in the National Comprehensive Cancer Network clinical guidelines, which recommend testing by next-generation sequencing (NGS) for those with nonsquamous NSCLC. But there’s high variability in what type of testing patients receive. Single gene vs NGS? DNA vs RNA? With the arrival of immunotherapy, what about immunohistochemistry screening to identify the presence of PD-L1 proteins? What about blood testing for circulating cell-free DNA?
“You would think that the vast majority of patients with NSCLC would have NGS testing,” Brandes said, because so many driver mutations have been identified and NGS can replace other types of testing.
But that’s not so. A study in JCO Precision Medicine found that only 54.7% of White patients with lung adenocarcinoma had testing performed.3 “Worse, it’s a significantly smaller percentage of [Black] patients” at 43.8%, he said.
“So this raises 2 issues in my mind,” Brandes said. “We’re not where we need to be in testing patients appropriately; 50% of patients do not get the appropriate testing. And then, the health disparities that are resulting from this—a substantially smaller percentage of [Black] patients being tested is also a real issue that needs to be tackled.”
Testing falls short even though lung cancer has more approved targets than other cancers, he said. Although EGFR and KRAS are the most common mutations, many less common ones now have therapies—and data show they work. Brandes shared a list of approved therapies and targets that filled 2 slides. “For the vast majority of patients, you have response rates in the first-line setting that are anywhere between 60% and 80%,” he said. “The duration of response is significantly longer than what you would expect from chemotherapy.”
KRAS, Immunotherapy, and More
Brandes briefly reviewed the parameters for using immunotherapy. “The big biomarker here is the PD-L1 expression level of greater than 50%,” he said. At that point, responses are “quite high,” although he noted that “in patients who have any level of PD-L1 expression, immunotherapy is approved.” In addition, for patients with low-expressing or no expression of PD-L1, “there seems to be synergy with chemotherapy,” he said.
He reviewed combinations involving a CTLA-4 inhibitor, such as adding the CTLA-4 inhibitor tremelimumab (Imjudo) to durvalumab (Imfinzi) and chemotherapy, which was tested in the phase 3 POSEIDON trial (NCT03164616).4 Brandes offered caution about cross-trial comparisons but said that the magnitude of benefits does not seem significantly higher than with a PD-L1 agent alone; he noted that there may be subgroups that benefit from these combinations.
“So what are the current challenges?” Brandes asked. He outlined several, as follows:
Drug resistance. Patients develop resistance to first-line tyrosine kinase inhibitor (TKI) treatment, and going to a different TKI is not an automatic option due to heterogeneous mechanisms of resistance; Secondary mutations occur in EGFR, such as MET overexpression. “The questions here become, ‘How do we deal with that if it happens, and how do we prevent it from happening?’ ” he noted.
Approaches to osimertinib resistance include combining the EGFR inhibitor with monoclonal antibodies, and the development of fourth-generation therapies. Brandes cited data from the phase 3 FLAURA2 study (NCT04035486), which found that EGFR inhibitor osimertinib (Tagrisso, AstraZeneca), combined with chemotherapy, produced 38% improvements in progression-free survival (PFS), or 8.8 months.5 “There didn’t seem to be a whole lot of synergistic toxicity between [osimertinib] and chemotherapy,” he said, noting that patients with central nervous system involvement benefited the most.
Targeting KRAS. Brandes said current challenges include improving on current KRAS data and moving KRAS inhibitors into the first-line setting. He mentioned data from the phase 2 KRYSTAL-7 study (NCT04613596) presented at the European Society of Medical Oncology Congress 2023, which showed combining pembrolizumab (Keytruda, Merck) with adagrasib (Krazati, Mirati) had promising results. In patients with PD-L1 up to 50%, the overall response rate was 63% and durable complete response was 83%.6
In the pipeline. What is the role of antibody-drug conjugates in lung cancer? After success in breast cancer, this class is crossing over. Brandes discussed sacituzumab govitecan (Trodelvy, Gilead) with pembrolizumab in the first-line setting. Results from the phase 2 EVOKE-02 trial (NCT05186974) showed an ORR of 69% in patients with PD-L1 above 50% and 44% in patients with PD-L1 below 50%.7 (Editor’s note: As this issue of Evidence-Based Oncology went to press, Gilead announced that the phase 3 EVOKE-1 trial [NCT05089734] failed to meet its primary end point. Although overall survival had improved by 3 months for patients who had not previously responded to a PD-L1 inhibitor, similar results were not seen in those who had a previous response to anti–PD-L1 treatment.8)
In the phase 3 TROPION-Lung01 trial (NCT04656652) of datopotamab deruxtecan, Brandes said there was “marginal” PFS improvement over docetaxel, “but subgroup analyses favor nonsquamous histologies.”9
Health Equity
Brandes concluded by asking the question he said “is probably most important”: How do we deal with health inequities? Hope for patients, he said, is tempered by the challenge of asking why NGS testing “is still lagging behind expectations.” There has been progress in the first-line setting, and the question now is how to “maximize these responses.”
However, he said, “You cannot benefit from targeted treatment or personalized treatment if you don’t know the genomic landscape of the malignancy you’re treating.”
References
1. Kanellakis NI, Jacinto T, Psallidas I. Targeted therapies for lung cancer: how did the game begin? Breathe (Sheff). 2016;12(2):177-179. doi:10.1183/20734735.006316
2. Kris MG, Johnson BE, Berry LD, et al. Using multiplexed assays of oncogenic drivers in lung cancers to select targeted drugs. JAMA. 2014;311(19):1998-2006. doi:10.1001/jama.2014.3741
3. Bruno DS, Hess LM, Li X, Su EW, Patel M. Disparities in biomarker testing and clinical trial enrollment among patients with lung, breast, or colorectal cancers in the United States. JCO Precis Oncol. 2022;6(6):e2100427. doi:10.1200/PO.21.00427
4. Johnson ML, Cho BC, Luft A, et al; POSEIDON Investigators. Durvalumab with or without tremelimumab in combination with chemotherapy as first-line therapy for metastatic non-small-cell lung cancer: the phase III POSEIDON study. J Clin Oncol. 2023;41(6):1213-1227. doi:10.1200/JCO.22.00975
5. Planchard D, Jänne PA, Cheng Y, et al; FLAURA2 investigators. Osimertinib with or without chemotherapy in EGFR-mutated advanced NSCLC. N Engl J Med. 2023;389(21):1935-1948. doi:10.1056/NEJMoa2306434
6. Garassino MC, Theelan WSME, Jotte R, et al. KRYSTAL-7: efficacy and safety of adagrasib with pembrolizumab in patients with treatment-naïve, advanced non–small cell lung cancer (NSCLC) harboring a KRAS G12C mutation. Presented at: European Society for Medical Oncology Congress 2023; October 20-24, 2023; Madrid, Spain. Abstract LBA65.
7. Garon EB, Liu SV, Owen SP, et al. EVOKE-2: a phase 2 study of sacituzumab govitecan (SG) plus pembrolizumab (pembro) with or without platinum chemotherapy in first-line metastatic non–small cell lung cancer (NSCLC). J Clin Oncol. 2022;40(suppl 16):TPS9146. doi:10.1200/JCO.2022.40.16_suppl.TPS9146
8. Gilead provides update on phase 3 EVOKE-01 study. News release. Gilead Sciences. January 22, 2024. Accessed January 23, 2024. https://bit.ly/3SqNjQd
9. Datopotamab deruxtecan improved progression-free survival vs chemotherapy in patients with previously treated non-small cell lung cancer in TROPION-Lung01 phase 3 trial. News release. AstraZeneca. October 23, 2023. Accessed January 23, 2024. https://bit.ly/3tX9Meu
Dr Kathy Zackowski Discusses the Importance of Rehabilitation Research and Trials in MS
April 26th 2024Kathy Zackowski, PhD, National MS Society, expresses the inherent value of quality rehabilitation trials for broadening clinical understandings of multiple sclerosis (MS) and bettering patient outcomes.
Read More
Mental Health Diagnoses, Care Challenges Rise Among US Youth, Report Finds
April 26th 2024While behavioral health care utilization has been rising, the treatment landscape has been worsening. New findings show that 20% of youths did not receive any form of treatment within 3 months of their initial behavioral health diagnosis.
Read More
Oncology Onward: A Conversation With Penn Medicine's Dr Justin Bekelman
December 19th 2023Justin Bekelman, MD, director of the Penn Center for Cancer Care Innovation, sat with our hosts Emeline Aviki, MD, MBA, and Stephen Schleicher, MD, MBA, for our final episode of 2023 to discuss the importance of collaboration between academic medicine and community oncology and testing innovative cancer care delivery in these settings.
Listen
