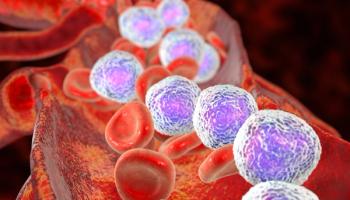
Acute Lymphoblastic Leukemia/Acute Myeloid Leukemia
Latest News
Latest Videos

Shorts
Podcasts
More News

Top articles in 2025 covered advancements in acute myeloid leukemia treatments, including allogeneic CAR T-cell therapy.

Blinatumomab enhances survival in pediatric B-cell ALL, yet homecare challenges hinder its outpatient delivery.

Financial and social barriers hinder access to specialized care and impact treatment outcomes for adolescents and young adults with leukemia.
Olutasidenib shows promising long-term efficacy and safety in treating relapsed or refractory mutant IDH1 acute myeloid leukemia.
Pretransplant NPM1 MRD testing significantly predicts relapse risk in acute myeloid leukemia.
Patients achieve a high 2-year survival and deep MRD-negative remissions with CAR T-cell therapy followed by stem cell transplant in B-cell ALL.

Research challenges age cut-offs in AML treatment, advocating for flexible, individualized approaches based on continuous age assessment.

The FDA approved ziftomenib for relapsed acute myeloid leukemia with NPM1 mutations, offering hope for high-risk patients.

Panelists discuss how venetoclax management requires standardized approaches to duration, bone marrow biopsy timing, growth factor use, and azole antifungal selection, with practices varying significantly between centers and the need for consistent protocols to optimize patient outcomes.

Panelists discuss how IDH inhibitors, particularly ivosidenib combined with azacitidine, represent potentially the greatest advance in AML treatment due to significant overall survival improvements, though adoption challenges include waiting for mutation results and limited patient applicability.

Guideline adherence in treating acute lymphoblastic leukemia (ALL) enhances health care resource utilization, especially for adolescent and young adult patients.

Panelists discuss how the treatment landscape has evolved from limited options to include hypomethylating agents and venetoclax combinations, with emerging oral formulations promising greater accessibility while requiring careful consideration of patient selection and toxicity management.

Panelists discuss how combination trials like VIALE-A and VIALE-C have demonstrated venetoclax’s survival benefits when added to hypomethylating agents, opening doors for numerous combination studies while emphasizing the need for randomized trials to prove clinical benefit in different disease contexts.

The FDA approved revumenib for relapsed/refractory (R/R) acute myeloid leukemia, offering a new targeted therapy option for patients with NPM1 mutations.

A novel combination therapy enhances the effectiveness of proteasome inhibitors against acute myeloid leukemia (AML), improving survival rates in preclinical models.

Panelists discuss how venetoclax has revolutionized AML treatment by providing effective therapy options for older patients with previously untreatable disease, enabling higher response rates, longer survival, and increased transplant eligibility while transforming the treatment landscape across all age groups.

Panelists discuss how transplant eligibility has expanded beyond traditional intensive chemotherapy candidates to include patients receiving lower intensity regimens, with earlier transplant consultations and consideration of organ function preservation through less toxic induction approaches.

Panelists discuss how current NCCN guidelines emphasize the importance of treating AML at experienced centers with proper infrastructure, while treatment decisions are based on intensive vs nonintensive therapy eligibility and specific genetic mutations like FLT3, IDH1, and TP53.

Panelists discuss how social determinants of health significantly impact AML care, particularly regarding transportation access, health literacy, and the intensive nature of treatment requiring frequent clinic visits for blood work and transfusions, which disproportionately affects patients living far from treatment centers.

A new drug application for Dasynoc, a lower-dose, bioequivalent formulation of dasatinib, was not approved for patients with chronic myeloid leukemia and acute lymphoblastic leukemia.

Experts discuss the importance of initiating blinatumomab treatment for acute lymphoid leukemia in academic centers for optimal patient care.

Panelists discuss how the greatest unmet needs include addressing poor outcomes in specific subsets like TP53-mutant disease, managing the increasingly older population with secondary mutations, and ensuring global access to targeted therapies and next-generation sequencing.

Panelists discuss how fitness assessment has evolved beyond traditional age cutoffs to incorporate comprehensive geriatric assessments, frailty measures, and individualized evaluations, while questioning whether intensive therapy should automatically be given to fit patients given newer effective treatment options.

Panelists discuss how current risk stratification systems, particularly the European Leukemia Net 2022 classification for intensive therapy and the 2024 classification for lower intensity treatments, categorize patients based on complex cytogenetics and molecular features to guide prognosis and treatment selection.

Panelists discuss how the pathophysiology of acute myeloid leukemia has evolved from a single phenotype understanding to recognizing diverse genetic events that lead to transformation at the hematopoietic stem cell level, with treatment decisions now increasingly integrated with specific genetic mutations despite the disease’s rapid progression timeline.