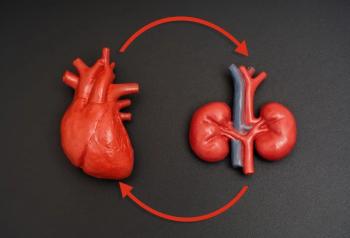
HIF Stabilizers: Management of Anemia in CKD
A review of data on daprodustat and vadadustat from randomized controlled trials in Japanese patients with anemia in CKD along with the clinical rationale for use of the HIF stabilizer class.
Transcript
Peter L. Salgo, MD: There are 2 other HIF [hypoxia-inducible factor] stabilizers. I’m going to try this now: daprodustat or daprodustat, I got both.
Daniel W. Coyne, MD: Daprodustat.
Peter L. Salgo, MD: Daprodustat and vadadustat. There are 2 studies there, right? They’re Japanese studies. What do they show?
Daniel W. Coyne, MD: We have information from these on ASN [American Society of Nephrology Kidney Week] presentations. The daprodustat study focused on looking at the safety of these agents. What they focused on was whether it was increasing cardiovascular events or death. They took 2 RCTs [randomized controlled trials]. One of these was an open-label study, and the other was a double-blind study, and they combined the safety data. They also focused on some concerns about activating HIF, in that, if you look at HIF activation, say within cancers, it may play a role in cancer growth. The thought was that, even though that’s very localized in the tissue, giving this HIF stabilizer could be adverse, and they looked at whether a cancer signal occurred. They also looked at ophthalmologic problems. In diabetic retinopathy, there’s demonstration of HIF activation playing a role there, so they had patients get ophthalmologic exams. Lastly, they looked at cardiovascular events.
What they saw when they combined these, which was over 1000 patients on either ESAs [erythropoietin-stimulating agents] or the HIF stabilizers was that there was no ophthalmologic signal. They saw adverse events in about 3% in both groups of patients. There was no cancer signal; less than 1% of patients were developing any cancer having progression issues. Ophthalmologic exams did not detect any difference between the 2 groups. Interestingly, cardiovascular events were a bit lower in the HIF stabilizer group at about 3% versus 6%. That was the safety study using daprodustat.
The other study by [Masaomi] Nangaku [MD, PhD,] was an efficacy study looking at vadadustat versus darbepoetin again, and this showed that it was just as efficacious. As Bob said, it works, so they looked at these patients not undergoing dialysis. They’re anemic, and some of them are anemic and on no therapy. They get put on either darbepoetin, or the HIF stabilizer, or vadadustat. They both have hemoglobin increases, and they both achieve goal at 20 to 24 weeks. Some of these patients were already on darbepoetin, and they would be re-randomized to either stay on it or go on the vadadustat, and again, it maintained their hemoglobin levels. These drugs are certainly as efficacious as what we’ve been using before.
Peter L. Salgo, MD: If I hear you correctly, they’re as efficacious, and their risk profile is better than the standard drugs you’ve been using to date?
Daniel W. Coyne, MD: I would say that we need more of these publications on these other agents, but the data to date is that they are as safe or safer depending on the population we’re looking at.
Peter L. Salgo, MD: If they’re as safe, let’s think to there and be very conservative. They’re as safe, and they’re as efficacious. Where do they fit into the armamentarium that you’ve got right now? In other words, when I hear as safe, OK, they’re about the same, and if they’re as efficacious, OK, they’re about the same. What’s the big deal? I know you guys are excited, so explain to me why you’re excited with these things.
Robert Provenzano, MD, FACP, FASN: Let me start. To address Dan’s point, he’s correct. These are as safe and at least as far as roxadustat, probably safer in some patients. It starts addressing the issues that we brought up earlier on our wish list. It’s easier for the patient to take, it’s more physiologic, you avoid high pharmacologic doses of ESAs that are potentially harmful themselves, it’s easy to store, and on and on and on. Roxadustat has been licensed in Japan and in China, and looking at how it’s being utilized there, it’s a fairly steady uptake. Physicians tend to be very conservative, and incremental information is going to be required for us to be comfortable. From a personal perspective, this offers an option that serves our patients’ needs and has huge upsides for us to better understand these small molecules.
There’s data out there that we presented at ASN that showed it may delay progression of renal function, so that’s a huge hit; it’s up to 20% to 25%. That’s enormous. It also significantly decreased LDL [low-density lipoprotein] cholesterol levels, so there is a huge opportunity there. To Dan’s point, we expect FDA approval probably in December of this year, but we still have a lot to learn. It’s a great opportunity for clinicians to start pressing this issue.
Peter L. Salgo, MD: If I hear you correctly, in addition to all of the hemoglobin issues, it decreases progression of renal disease and improves your cholesterol profile, which may or may not spare you the use of a statin, for example. Those are big advantages.
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.