News
Article
Incremental Effectiveness, Costs May Improve Using Biomarker-Guided Selection
Author(s):
Lowered costs and incremental effectiveness could improve when using biomarker-guided selection for treatment of patients with metastatic colorectal cancer using first-line nivolumab.
Choosing the patients who should be treated with first-line nivolumab, a PD-1 inhibitor, by using a selection guided by biomarkers could help to reduce costs and improve efficacy of the treatment in patients with microsatellite stable (MSS)/proficient mismatch repair (pMMR) metastatic colorectal cancer (mCRC), according to an abstract presented at European Society for Medical Oncology Congress 2024 by Benjamin Geisler, MD, MPH.
Nivolumab has been an emerging first-line treatment when added to cytotoxic chemotherapy, specifically in patients with MSS/pMMR mCRC. According to Geisler, a METIMMOX study published in 2024 found that there were no significant differences when alternating 2 cycles of oxaliplatin-based chemotherapy (FLOX) and 2 cycles of nivolumab compared with FLOX alone for the primary endpoint of progression-free survival (PFS). However, several biomarker-determine subgroups were able to show a reduction. This abstract aimed to compare the price of using FLOX by itself with alternating FLOX and nivolumab with 2 cycles each when treating MSS/pMMR mCRC, both with and without the selected biomarker subgroups.
A partitioned survival model was developed using the individual participant data from the phase 2 randomized controlled trial, METIMMOX-1. This was done by fitting both PFS and overall survival in parametrically. Surveys were given to all participants to assess their health-related quality of life and health care costs were estimated in 2023 Euros. Costs included second-line care and end-of-life care, along with other drugs and tests.
The incremental cost-effectiveness ratio (ICER) was estimated for all patients and subgroups using cut-offs. These included at least 10% target lesion reduction after the first radiographic reassessment, tumor mutational burden (TMB) of more than 8.0 mut/MB, and C-reactive protein of less than 5.0 mg/L when starting nivolumab. All outcomes were discounted 4% per year.
“We used those discounted costs and overall survival with adjustment for quality of life to estimate an [ICER] and compared it to the threshold of around €51,000,” said Geisler. “This is a specific Norwegian threshold based on the reduction of quality adjusted life years by [mCRC]. So below the threshold, treatments would generally be considered cost effective in Norway for this specific indication.”
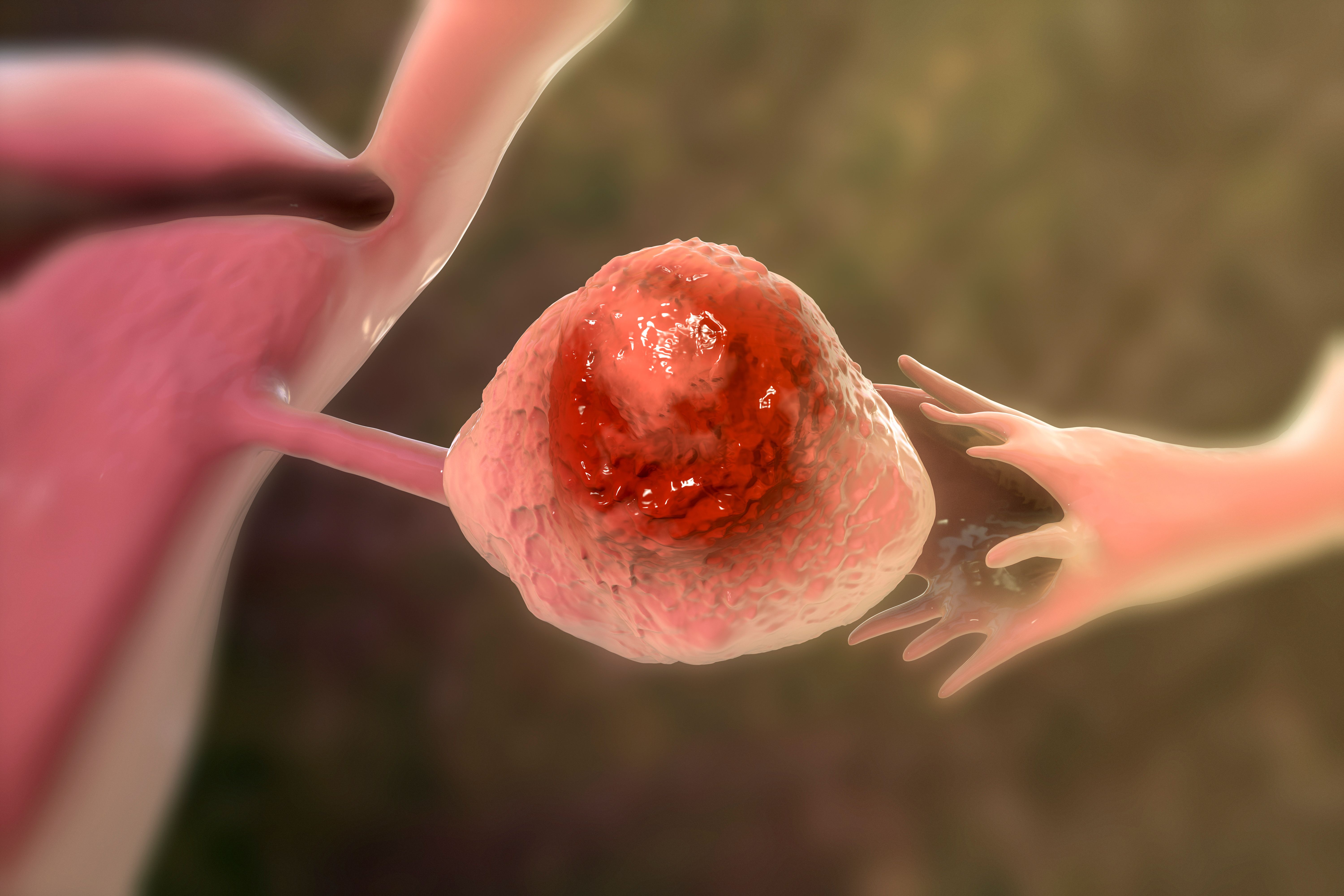
Using specific biomarkers to determine treatment could improve cost and quality of life in patients with metastatic colorectal cancer | Image credit: Stillfx - stock.adobe.com

Geisler presented baseline characteristics and key input paramaters that estimated that the cost per FLOX cycle was €427 and the cost per nivolumab cycle was €13,923. The estimated mean cost of the last month of a patient’s life was estimated at €13,803 and cost for next generation sequencing was €1439.
There were 76 patients included in the study, of which 46.1% were women and the overall median (IQR) age was 64.5 (57.8-72.0). The median tumor lesion reduction after 2 plus 2 cycles was 24%. The TMB was only calculated for the experimental arm as of the presentation, with the control arm still needing to be calculated.
Quality adjusted life years (QALYs) provided by adding nivolumab to all patients equaled 0.1175 while also having incremental costs of more than €75,000. The ICER in this case would not be cost-effective overall, at 638,798, as the treatment would be used in all patients. Lower ICERs were achieved when using biomarkers to select the eligible patients for the treatment. This was able to double or triple incremental QALYs and lower the incremental costs.
This is demonstrated when separating the subgroups out and looking at the incremental costs and QALYs for each subgroup chosen to alternate FLOX and nivolumab. Those who are in the subgroup of target lesion reduction of 10% or more, the incremental costs were reduced to €30,386, QALYs increased to 0.2112, and ICER decreased to 143,850. Similar trends were found in the subgroup with C-reactive protein of less than 5.0 mg/L, where the incremental costs were €32,945, QALYS were 0.2920, and ICER was 112,840, and in the subgroup looking for TMB of more than 8.0 mut/MB, where incremental costs were reduced to €14,490, the QALYs were 0.3377, and the ICER was 45,451.
“While the additional costs for the anti-PD-1 strategy was lower for the biomarker guided strategies…the quality gain was higher, maybe because patients were better selected by these biomarkers. This resulted then in lower ICERs,” said Geisler.
There were some limitations to this study. The analyses was a post-hoc analysis and based on post-hoc data. The control group lacks TMB data. A probabilistic sensitivity analysis needs to be conducted, as Geisler noted that it would help to determine the effect that the small sample size had on the results of the study. The results are also dependent on Norwegian costs, which may make it less generalizable to other parts of the country.
“Biomarker guided selection for anti-PD-1 compared to treating all metastatic MSS patients may improve its clinical effectiveness while lowering costs, making it potentially cost effective, at least in Norway,” Geisler concluded. “In particular the value of a [TMB] strategy is promising, and prospective validation should strongly be considered.”
Reference
Geisler BP, Meltzer S, Burger EA, Aas E, Ree AH. Value of immune checkpoint blockade (ICB) in microsatellite stable:mismatch repair proficient (MSS:pMMR) metastatic colorectal cancer (mCRC). Presented at European Society for Medical Oncology Congress 2024; September 13-17, 2024; Barcelona, Spain. Abstract 1537O.
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.

The Importance of Examining and Preventing Atrial Fibrillation