Payer Perspective of HIF Stabilizers for Anemia in CKD
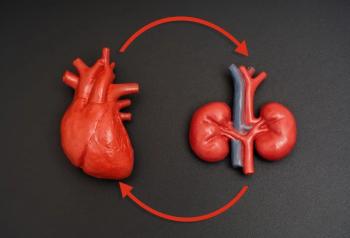
A payer perspective of factors to consider when creating drug policies for HIF stabilizers for patients with anemia in CKD.
Transcript
Peter L. Salgo, MD: Let me turn this over to Dr Crittenden. What does this cost? Are you going to start paying for this? In terms of step therapy, where does this fit? How do you go about this? It’s a new drug.
Stanley Crittenden, MD: Yeah, that’s the question. As a nephrologist, I’m also excited about this drug, but most health plans start the evaluation process for pipeline drugs way in advance of when NDA [new drug approval] are due for them. We’ve known about these drugs in the pipeline for a while. The drug evaluation process is very dynamic and diverse, but before I talk about that exact process, I’d like to spend a couple of seconds talking about how we think about drug utilization. The main purpose of a pharmacy utilization program is mainly to help us ensure that our patients are using the right drug at the right time. That is correct timing, the correct dosing, the correct route of administration, and the correct site of administration. Is this home, is this oral, is this office, is this infusion center, etc? Ultimately, you want to make sure that the patients are getting clinically proven, based on evidence, large randomized controlled trials—medications that are going to work for their condition.
The 3 most common utilization management strategies or tactics that you’ll see from almost all payers, which includes Medicare, Medicaid, and commercial type plans, are things like prior authorizations, step therapy, and quantity limits. Prior authorization is sometimes seen as the bane of a physician’s existence, but all we’re doing is asking for a preapproval for certain medications before they’re covered. What that does is it helps us understand how the patient is going to get the drug and if it’s going to be used safely and effectively. This, in turn, helps reduce things like inappropriate utilization. For example, in anemia of CKD [chronic kidney disease], this prior authorization process will help us drive to ensure that clinical best practices and standards are adhered to. For example, we mentioned earlier that we’re not giving ESAs to patients with cardiovascular risks.
Step therapy is another lever that plans will use to help with medication therapy management. The whole point of this is that you’ll have a patient or a member step through an initial drug before a non-preferred or noncovered drug is covered, although the preferred drug that you’re stepping through is usually of the same class or some mechanism of action or is generic—not always, but it’s often generic. It’s also seen as a widely safe, effective, and evidence-based standard of practice. For example, in the anemia realm, a lot of health plans may have preferred Retacrit [epoetin alfa-epbx], which is an epoetin-alpha biosimilar, and you’ll step through that before using the other Epogen [epoetin alfa] brands.
The final tactic or lever would be quantity limits. Quantity limits are just that: we don’t want to have patients out there with a 3-month supply of a drug that can be potentially dangerous that they don’t preserve or store properly. Patients can also inadvertently take higher doses, so we want to quantity limit patients so that you’re ensuring that the drug is appropriately used and stable.
To get back to how we’ll think about this new class of drugs, I’m excited about this possibility, and most plans have already looked at these drugs in the pipeline for quite some time. We’ll review lots of data points. For example, all these trials that both Dan and Bob mentioned, we’ll review all the relevant clinical literature. Health plans also love health outcomes or pharmacoeconomic studies to help us understand total cost of care. We’ll also consider what the current toolbox is. How is the new therapy going to help change management? Will it increase safety profile, or will it make it so that patients are now getting drugs and less advanced care or settings? For example, will this take a patient out of the hospital or infusion suite and keep them at home?
We look at things like whether it will drop the rate of red blood cell transfusions. Will it lower IV [intravenous] iron infusions because we know IV iron has its own set of challenges in terms of site of delivery and even adverse effects. Then with this new class of drugs, the signals in the literature that are showing slowing to kidney progression are important to know because we know that, if you slow the kidney progression, 1 less month on dialysis is much better in terms of patient quality of care and then total cost of care.
We always want to make sure that we’re standing in lock step with typical standard-of-care, health care community medical practice. I can’t say this enough: the health plan’s job is to make sure that for our physician partners in the community, we’re practicing contemporary evidence-based medicine that is standard of care.
Peter L. Salgo, MD: Whenever I see -stat on a drug name, I see dollar signs. They’re new, there’s a lot of money invested in them to bring them to market, and they’re expensive at least at first. What kind of data are you looking for to justify them financially?
Stanley Crittenden, MD: Good question. It comes down to cost, right? A lot of the time, you’ll see drug companies soon after the NDA is released, starting the pharmacoeconomic studies to help understand total cost of care. They will perhaps have their drug to say reduction in hospitalization or something like that, so that the plan will understand the total collective value.
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.