- January 2024
- Volume 30
- Issue 1
- Pages: SP71-SP72
Subcutaneous Epcoritamab Brings 82% Overall Response in Patients With R/R Follicular Lymphoma
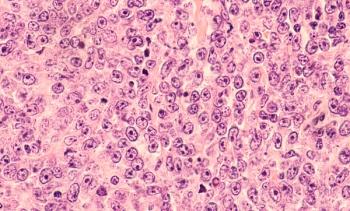
Epcoritamab, already approved as Epkinly to treat patients with certain types of large B-cell lymphoma, produced strong overall responses in patients previously treated with at least 2 therapies for follicular lymphoma (FL). The results, which were first round of data from an expansion cohort of EPCORE-NHL-1 (NCT03625037) for patients with FL, were presented December 9, 2023, at the 65th American Society of Hematology (ASH) Annual Meeting and Exposition in San Diego, California.1
Officials from AbbVie and Genmab, developers of epcoritamab, announced before ASH that FDA had granted the bispecific antibody Breakthrough Therapy Designation in FL.2 The development means another CD3 x CD20-directed therapy, a T-cell engager, could be joining a competitive landscape in FL. Mosunetuzumab (Lunsumio; Genentech) is already approved,3 and the investigational therapy odronextamab (Regeneron) has a March 2024 deadline for FDA action.
Trial. The EPCORE-NHL-1 trial is a 3-part study to evaluate epcoritamab across multiple subtypes of non-Hodgkin lymphoma (NHL). The first part is the dose escalation phase, the second is a phase 2a expansion study, and the third is a phase 2a dose optimization part. In phase 2a, additional patients were added to expansion cohorts in specific NHL subtypes, including FL. Dose optimization allows for adjustments to step-up regimens to limit effects of cytokine release syndrome (CRS).1,2 The primary end point is overall response rate (ORR); secondary end points are complete response (CR), duration of response (DOR), duration of complete response (DOCR), progression-free survival (PFS), and time to response. Overall survival, time to next therapy, and measures of minimal residual disease (MRD) are also being revaluated.
Patients with CD20-positive R/R FL who had received at least 2 prior lines of systemic treatment received subcutaneous (SC) epcoritamab in step-up doses in cycle 1, followed by full doses in 28-day cycles: doses were given weekly in cycles 1 through 3, every 2 weeks in cycles 4 through 9, and every 4 weeks through cycle 10 or until disease progression or unacceptable toxicity.
Results. Through October 2022, investigators enrolled 128 patients with R/R FL who met eligibility criteria to be treated with epcoritamab SC. Median age was 65 years, 85% were stage III or IV, and 61% of patients met high-risk criteria. Median prior number of therapies was 3, and 31% had at least 4 prior therapies; 19% had autologous stem cell transplant. As of April 21, 2023, the median follow-up was 17.4 months, and results were as follows1:
- ORR was 82%, with CR of 63%.
- Median time to response was 1.4 months, and median time to CR was 1.5 months.
- Both overall and complete responses were consistent across high-risk subgroups, including patients who were double refractory (76% ORR, 56% CR), and refractory to their last treatment (74% ORR, 51% CR).
- There was a trend toward higher response rates in earlier lines of treatment; those with 2 prior therapies had 89% ORR and those with 4 had 68%.
- Median PFS was 15.4 months and median DOR and duration of CR were not reached. An estimated 85% of patients remained in CR at 12 months.
- MRD negativity was correlated with improved PFS.
Safety. Common treatment emergent adverse events (TEAEs) were CRS of any grade (66%), injection-site reactions (57%), COVID-19 (40%), fatigue 30%), neutropenia (28%), and diarrhea (27%). Most CRS events were grade 1 (40%); 2% were grade 3. Most CRS events followed the first dose and none led to discontinuation. Eight patients reported immune effector cell–associated neurotoxicity syndrome (ICANS), and all cases resolved without discontinuation.
Thirteen patients (10%) died from TEAEs. In their abstract, the authors said the optimized regimen to reduce CRS risk did work to limit incidence and severity; in all, 19% of patients stopped treatment due to TEAEs.1 Still, the authors stated, the overall tolerability of epcoritamab in the dose-optimized group suggests this strategy could allow treatment in an outpatient setting.2
“Despite treatment advances for patients with follicular lymphoma whose disease has unfortunately progressed, treating relapsed or refractory follicular lymphoma remains highly challenging, particularly as a third-line treatment,” investigator Catherine Thieblemont, MD, PhD, head of the hemato-oncology department, Paris University, Hôpital Saint-Louis Assistance-Publique-Hôpitaux de Paris, said in a statement.
“The patients in this trial represent a historically difficult-to-treat patient population,” she continued, calling the data “especially notable” because the study reported “high overall and complete response rates for this investigational therapy and a preview for its potential as a treatment option.”2
References
- Linton K, Jurczak W, Lugtenburg P, et al. Epcoritamab SC monotherapy leads to deep and durable responses in patients with relapsed or refractory follicular lymphoma: first data disclosure from the EPCORE NHL-1 follicular lymphoma dose-expansion cohort. Presented at: 65th American Society of Hematology Annual Meeting and Exposition; December 9-12, 2023; San Diego, CA: Abstract 1655. https://ash.confex.com/ash/2023/webprogram/Paper179887.html
- New data for bispecific antibody epcoritamab (DuoBody CD3xCD20) shows strong, durable treatment response for patients with difficult-to-treat relapsed/refractory (R/R) follicular lymphoma (FL). News release. AbbVie. December 9, 2023. Accessed January 2, 2024.
https://prn.to/4aFauNQ - FDA grants accelerated approval to mosunetuzumab-axgb for relapsed or refractory follicular lymphoma. FDA. December 23, 2022. Accessed January 2, 2024.
https://bit.ly/3kGqud1
Articles in this issue
about 2 years ago
Overcoming Barriers to Care Equity in Multiple Myelomaabout 2 years ago
ASH 2023: Coverage in MDS, Myeloproliferative Diseaseabout 2 years ago
ASH 2023: Coverage in Multiple Myelomaabout 2 years ago
ASH 2023: Coverage of ALLabout 2 years ago
ASH 2023: Coverage of cHLabout 2 years ago
ASH 2023: Coverage of MCLabout 2 years ago
ASH 2023: Coverage of CLL/SLLabout 2 years ago
ASH Abstracts Showcase Effective Treatments for MM, CLL, FLabout 2 years ago
Data Reveal Racial, SDOH Factors Linked to OS Differences in CLLNewsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.