News
Article
Tarlatamab Receives Accelerated Approval for Extensive-Stage SCLC
Author(s):
The FDA has approved tarlatamab (Imdelltra; Amgen), a novel bispecific T-cell engager, to treat patients with extensive-stage small cell lung cancer (SCLC).
Tarlatamab has been granted accelerated approval for patients with extensive-stage small cell lung cancer.
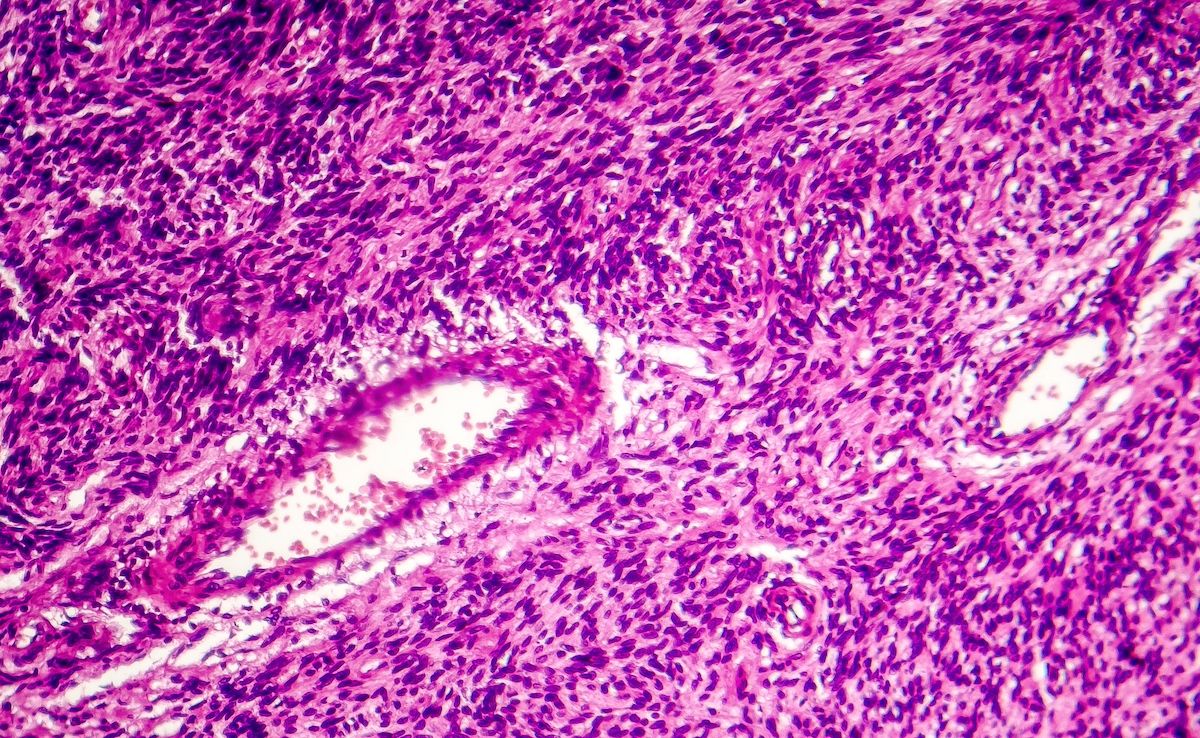
Image credit: wladimir1804 - stock.adobe.com

The FDA granted accelerated approval for tarlatamab-dlle (Imdelltra; Amgen) to treat patients with extensive-stage small cell lung cancer (ES-SCLC) who experience disease progression on or after platinum-based chemotherapy.1 The approval comes a month ahead of the June 12 action date.2
Tarlatamab is a bispecific T-cell engager that latches onto tumor cells and immune cells at the same time, bringing them close together to help the T cell recognize and destroy the cancer cell.3
"The FDA's approval of Imdelltra marks a pivotal moment for patients battling ES-SCLC. This DLL3-targeting therapy in ES-SCLC comprises a transformative option demonstrating long-lasting responses in pretreated patients," Jay Bradner, MD, executive vice president, Research and Development, and chief scientific officer at Amgen, said in a statement.4 "Imdelltra offers these patients who are in urgent need of new innovative therapies hope, and we're proud to deliver this long-awaited effective treatment to them."
The efficacy of tarlatamab was evaluated in 99 patients in the phase 2 DeLLphi-301 trial (NCT05060016), an open-label, multicenter, multicohort study of patients with relapsed/refractory ES-SCLC with disease progression after platinum-based chemotherapy.1
The overall response rate (ORR) per RECIST 1.1 was 40% (95% CI, 31%-51%) and the median duration of response was 9.7 months (range, 2.7-20.7+). There were 69 patients with data regarding their platinum sensitivity status. The ORR was 52% (95% CI, 32%-71%) in 27 patients with platinum-resistant SCLC and 31% (95% CI, 18%-47%) in 42 patients with platinum-sensitive SCLC.
"Lung cancer is a complex and devastating disease, and less than 3% of patients with ES-SCLC live longer than 5 years," said David P. Carbone, MD, PhD, professor of internal medicine and director of the James Thoracic Oncology Center at the Ohio State University Medical Center.4 "In the DeLLphi-301 trial, the median overall survival was 14.3 months, with 40% of patients responding to treatment with tarlatamab. These responses were remarkably durable, representing a major advancement in the SCLC treatment paradigm."
The full results of the phase 2 DeLLphi-301 study were published in The New England Journal of Medicine.5 In part 1, 88 patients received a 10-mg dose of tarlatamab and 88 patients received a 100-mg dose. The median progression-free survival was 4.9 months (95% CI, 2.9-6.7) in the 10-mg group and 3.9 months (95% CI, 2.6-4.4) in the 100-mg group.
The most common adverse events were cytokine-release syndrome (CRS; 51% in the 10-mg group and 61% in the 100-mg group), decreased appetite (29% and 44%, respectively), pyrexia (35% and 33%), constipation (27% and 25%), and anemia (26% and 25%). Eleven (8%) patients in the 10-mg group and 24 (28%) patients in the 100-mg group experienced Immune effector cell-associated neurotoxicity syndrome (ICANS) and associated neurologic events.
The median (IQR) time from most recent tarlatamab dose and onset of CRS was 13.1 hours (7.8-27.4), and the median duration of CRS was 4 days (2-6).
Tarlatamab has a Boxed Warning for CRS and neurologic toxicity, including immune effector cell–associated neurotoxicity syndrome.
"After decades of minimal advancements in the SCLC treatment landscape, there is now an effective and innovative treatment option available," said Laurie Fenton Ambrose, cofounder, president, and CEO of GO2 for Lung Cancer.4 "Today's FDA approval marks a significant milestone for the SCLC community as the availability of a targeted bispecific therapy brings forward new possibilities to those living with this aggressive disease."
Since the approval of tarlatamab was granted under the accelerated approval pathway, continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial.
References
- FDA grants accelerated approval to tarlatamab-dlle for extensive stage small cell lung cancer. News release. FDA. May 16, 2024. Accessed May 16, 2024. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-tarlatamab-dlle-extensive-stage-small-cell-lung-cancer
- FDA grants priority review to Amgen's tarlatamab application for advanced small cell lung cancer. News release. Amgen. December 13, 2023. Accessed May 16, 2024. https://www.amgen.com/newsroom/press-releases/2023/12/fda-grants-priority-review-to-amgens-tarlatamab-application-for-advanced-small-cell-lung-cancer
- Ben-Ari E. Tarlatamab shows promise for some people with small cell lung cancer. National Cancer Institute. December 1, 2023. Accessed May 16, 2024. https://www.cancer.gov/news-events/cancer-currents-blog/2023/tarlatamab-previously-treated-sclc
- FDA approves Imdelltra (tarlatamab-dlle), the first and only T-cell engager therapy for the treatment of extensive-stage small cell lung cancer. News release. Amgen. May 16, 2024. Accessed May 16, 2024. https://www.amgen.com/newsroom/press-releases/2024/05/fda-approves-imdelltra-tarlatamabdlle-the-first-and-only-tcell-engager-therapy-for-the-treatment-of-extensivestage-small-cell-lung-cancer
- Ahn MJ, Cho BC, Felip E, et al; for the DeLLphi-301 Investigators. Tarlatamab for patients with previously treated small-cell lung cancer. N Engl J Med. 2023;389(22):2063-2075. doi:10.1056/NEJMoa23079