Video
Role of Anemia in CKD
Peter L. Salgo, MD: We’re going to be talking about anemia here. What percentage of the chronic kidney disease [CKD] population gets anemic, and what is the etiology of the anemia?
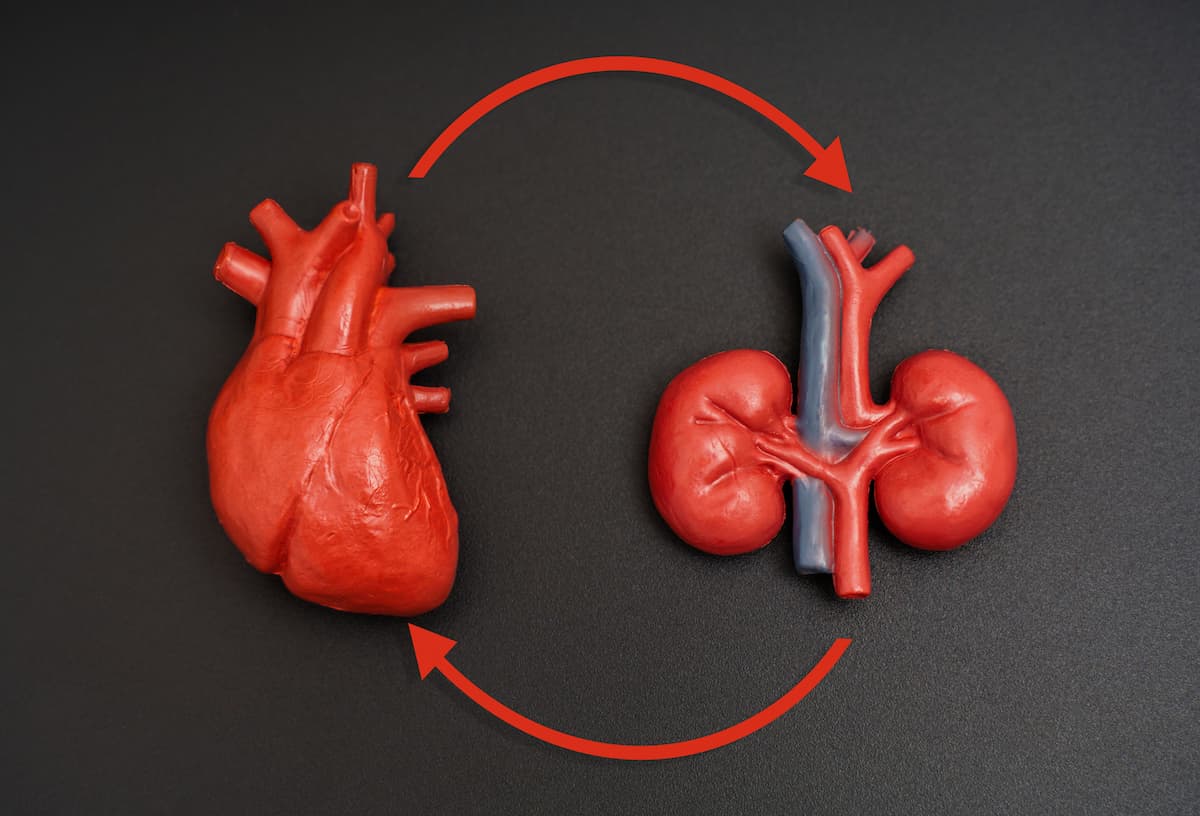
Robert Provenzano, MD, FACP, FASN: As Dan and I mentioned, the worse your kidney function, the more likely you are to be anemic. As we move through the stages, in CKD stage I and II, it is very unusual to be anemic. Indeed, if you are anemic, you should look for other causes. The anemia focuses on the kidney because it’s the erythropoietin-producing cells within the kidney that produce erythropoietin, which then stimulates the bone marrow to make red blood cells. As you progress through stages III and IV, in stage III, about 5% patients are anemic. In stage IV, it is 40%. By the time you’re at stage V and ready to progress to kidney failure, it’s as high as 70%. This is something we track closely because there are management opportunities there.
Peter L. Salgo, MD: This is my opportunity to ask you guys, because when I was your age—actually I’m old—we always called something the anemia of chronic disease. I noticed that it was always associated or often associated with renal disease. People who were chronically ill had renal complications, and they were also anemic. I know there’s some bone marrow involvement, but isn’t the anemia of chronic disease an erythropoietin-related, renally related consequence of chronic disease? Am I wrong? Anybody want to tackle that? It’s unfair.
Daniel W. Coyne, MD: I would probably put it the other way: The anemia of chronic kidney disease in part is due to the anemia of chronic disease. Chronic inflammation emulates IL-6 and other factors that affect erythropoiesis, and we may talk about this later. It increases a protein called hepcidin, which regulates iron absorption and iron availability, and that’s the anemia of chronic disease.
You can imagine that you can have it in somebody with rheumatoid arthritis because they’re inflamed with normal kidney function. CKD is an inflammatory state as well, so we see lots of inflammatory markers in the patients, and it is driving a great deal of the anemia that we see.
Peter L. Salgo, MD: Is there a specific risk factor for anemia in CKD, or is it just all across the board?
Daniel W. Coyne, MD: Diabetes. If you have the presence of diabetes, you’re far more likely to be anemic, and it’s far less likely to resolve if we observe it over the next 90 days.
Peter L. Salgo, MD: Once you get anemic in the presence of chronic kidney disease, how does the anemia per se impact patients’ lives?
Robert Provenzano, MD, FACP, FASN: Let me start for that, because this is a controversial issue. In the last 30 years, a lot of focus has been on the impact of anemia on the quality of life, and many trials that we’ll address later have tried to look at advantages of normalizing hemoglobin, or at least pushing your hemoglobin levels toward normal: 11.0, 11.5 g/dL. However, there’s anecdotal evidence that individual patients feel better: All of us have our stories about an accountant or a professor who had a hemoglobin of 9.0 g/dL and couldn’t function, and their hemoglobin went up to 11.0 g/dL, and they felt fantastic. The large trials have not shown a direct impact on quality of life. That being said, there are physiological advantages of getting hemoglobin levels above 10 g/dL.
Peter L. Salgo, MD: There’s a distinction, it seems to me as a clinician, between where you should transfuse to in an acute state and where people work best. In other words, they came out of the open-heart operating room with a hematocrit of 20%. We would have cranked him up to 30% in the past, but the data show that they don’t do better from a cardiovascular perspective. On the other hand, what I hear you saying is that they do better for life with better hematocrit.
Robert Provenzano, MD, FACP, FASN: I’ll start and then hand it to Dan. We need to distinguish between acute anemia and chronic anemia.
Peter L. Salgo, MD: Yes.
Robert Provenzano, MD, FACP, FASN: In a chronic state, think there are opportunities for improvement of quality of life. In the acute phase, particularly if it’s a relatively healthy individual without CKD, they can certainly manage their anemia. Dan, feel free—I didn’t mean to cut you off.
Daniel W. Coyne, MD: You need to remember that CKD generally presents in older people and people with diseases; they tend to be more sedentary. When they get anemic, the anemia is not limiting their oxygen delivery. They’re never pushing it to a point where they need that extra oxygen. It’s different if you’re an NBA [National Basketball Association] player. If you’re an NBA player with kidney transplant, then you’re going to need some erythropoietin to get to a normal hematocrit and function. In reality, that’s not who we treat. I do see people in their 30s and 40s who are very active and have CKD, and they seem to function much better when their hemoglobin is normal or near normal, and they seem to be affected even when it’s in the 10s. Most of my patients don’t feel any different in the high 9s or 11s, and that’s what the trials were looking at: those types of patients.
Peter L. Salgo, MD: Does the staging of CKD depend on anemia? Is that part of your equation?
Robert Provenzano, MD, FACP, FASN: No.
Daniel W. Coyne, MD: No.
Robert Provenzano, MD, FACP, FASN: The staging is related solely to the EGFR [estimated glomerular filtration rates]. In other words, how severe the disease has progressed.
Peter L. Salgo, MD: Let me turn it the other way; let me turn it upside down. In which stage of CKD does anemia begin to play an important part?
Robert Provenzano, MD, FACP, FASN: I would think stage IV. Go ahead, Dan.
Daniel W. Coyne, MD: I would say in stage IIIB we start to see a minority of patients for whom it’s clearly a problem, but it’s mostly stage IV CKD, which is less than 30% renal function.
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.