News
Article
Visual Acuity, Retinal Sensitivity Improved With Intravitreal Ranibizumab Injection
Author(s):
An intravitreal ranibizumab injection was able to improve retinal sensitivity and thickness along with improving visual acuity.
Visual acuity improved significantly over a 6-month period when patients received intravitreal ranibizumab injections (IRI), according to a study published in the Journal of Clinical Medicine.1 Retinal sensitivity and thickness also improved in most or all of the retinal regions when using the treatment in patients who had good or poor improvements in best corrected visual acuity (BCVA).
Branch retinal vein occlusion (BRVO) can affect people aged 40 years and older and can occur due to a patient living with other diseases related to their lifestyle, including hypertension. There are approximately 13.9 million people across the United States, Europe, Asia, and Australia who have diagnosed BRVO and 16.4 million affected by RVO as of 2011.2 Macular edema acts as the biggest threat to vision in patients with BRVO and can be measured through retinal sensitivity and visual acuity.
The study aimed to assess the changes in patients’ eyes, specifically in their visual acuity, retinal sensitivity, and retinal thickness, when using IRI for the treatment of macular edema in BRVO.
Patients who were treatment-naïve and had visual impairment related to BRVO and macular edema at the Tokyo Medical University in Tokyo, Japan, were considered for the study. Patients who were older than 30 years, had no prior history of ocular treatment, had a central macular thickness (CMT) of 300 μm or higher, were examined within 3 months of their first symptoms, and had a period of follow-up after their IRI treatment of at least 6 months were included in the study. Patients that had a separate ocular disorder, had fundus laser therapy or anti-vascular endothelial growth factor (VEGF) treatment in the past, had a history of eye surgery, or had an eye disease that could affect vision were excluded from the study.
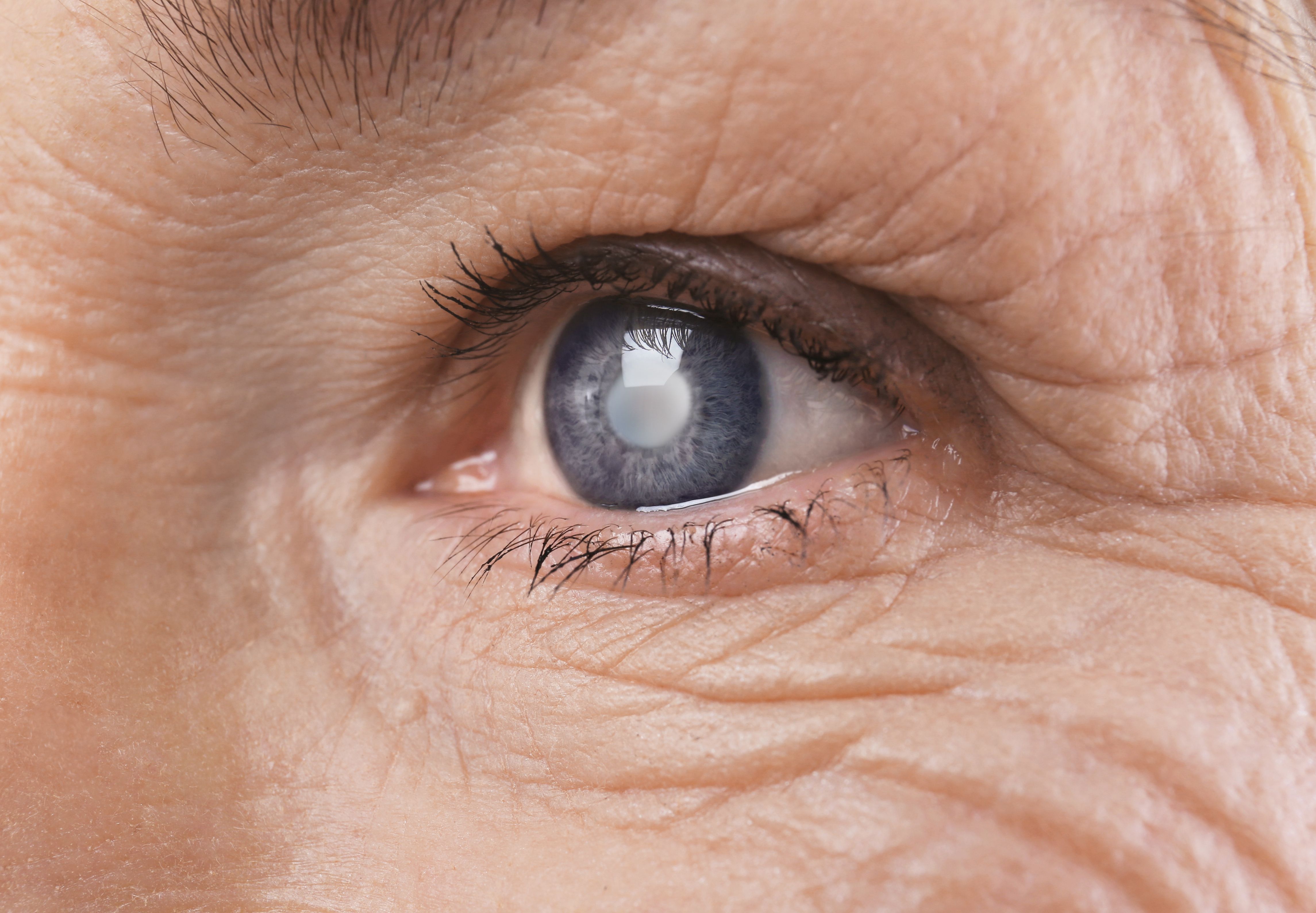
Retina and optic nerve | Image credit: memorisz - stock.adobe.com

The diagnoses were confirmed prior to treatment with IRI. Optical coherence tomographies were collected from all participants to determine if serous retinal detachment (SRD) was present and to calculate CMT. All participants had a microperimetry performed, which is a combination of automated perimetry and digital fundus imaging. These were done at baseline and monthly for the next 6 months. A retinal sensitivity map was created through the use of an MP-3 microperimeter.
The study included 34 eyes from 34 patients who had macular edema due to BRVO. Occlusion of the superior vein was found in 19 participants and occlusion of the inferior vein was found in 15. Systemic hypertension was present in the majority of the patients, and SRD was present in half of the patients before IRI, which was reduced to 23.5% after 6 months.
There mean (SD) number of IRIs was 2.7 (0.9) after 6 months, and BCVA improved from 0.13 (0.18) after 1 month of follow-up to 0.14 (0.25) after 6 months of follow-up. Retinal thickness in all 9 macular subfields improved significantly during the follow-up, whereas retinal sensitivity improved in 8 retinal regions.
Retinal thickness improved in all 9 macular subfields over time in patients who had both good improvement in BCVA and used IRI, and it improved in 8 subfields in patients with poor improvement in BCVA, with a reduction in μm found in all subfields after 6 months (P = .014 in the outer non-occluded subfield; P < .001 in all remaining subfields).
Significant differences were found between patients with good and poor improvement in BCVA when it came to retinal sensitivity. The non-occluded region was the only region that was not significantly improved in terms of retinal sensitivity in patients with good improvement in BCVA after using IRI (P = .176 in outer non-occluded region; P < .001 for all remaining regions); patients with poor improvement in BCVA only had improvement in sensitivity in 6 regions.
Mean age (59.4 [9.1] years vs 64.8 [9.8] years), sex (10 men and 8 women vs 6 men and 10 women), duration of macular edema (28.1 [20.8] days vs 46.0 [33.4] days), mean number of IRIs (2.6 [1.0] vs 2.9 [0.7]), and prevalence of SRD (8 of 18 patients vs 9 of 16 patients) were not significantly different between the groups who had good improvement vs poor improvement.
There were some limitations to the study. The follow-up period was short and the data were retrospective. The sample size was small, which could have led to a lack of power behind the numbers. A singular anti-VEGF treatment was studied in this analysis; future studies should explore other types of anti-VEGF treatment. Optical coherence tomography could not accurately assess the changes in external limiting membrane and ellipsoid zone. Vision-related quality of life and associations between retinal sensitivity and quality of life should also be studied further.
IRI could significantly improve visual acuity over the course of 6 months as well as improve retinal thickness in 9 retinal regions and sensitivity in most retinal regions. IRI was also found to have a positive effect on retinal sensitivity and thickness in patients with poor improvement in BCVA. These effects could vary by retinal site, and visual improvement should be monitored closely while using IRI.
References
- Nonaka R, Noma H, Yasuda K, Sasaki S, Goto H, Shimura M. Visual acuity and retinal thickness and sensitivity after intravitreal ranibizumab injection for macular edema in branch retinal vein occlusion. J Clin Med. 2024;13:2490. doi:10.3390/jcm13092490
- Rogers S, McIntosh RL, Cheung N, et al. The prevalence of retinal vein occlusion: pooled data from population studies from the United States, Europe, Asia, and Australia. Ophthalmology. 2010;117(2):313-319.e1. doi:10.1016/j.ophtha.2009.07.017
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.