CMS Finalizes Kidney Care Model to Promote Home Dialysis, Live Donor Transplants
Trump administration officials said the new payment incentives represent the biggest change in kidney care in decades.
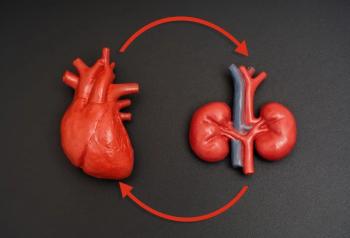
CMS today finalized a new payment model it said would give patients greater access to home dialysis and kidney transplants from live donors, which officials said would improve outcomes and quality of life while saving Medicare $23 million over 5 years.
Trump administration officials said
The End-Stage Renal Disease (ESRD) Treatment Choices (ETC) Model will be mandatory for 30% of kidney care providers—down from the 50% first proposed—and affect beneficiaries in all 50 states and the District of Columbia. A coalition of patient groups and dialysis providers and manufacturers warned that while CMS made some useful changes to its initial plan, some patients may still feel pushed into home care, and those who stick with dialysis centers may be at a disadvantage.
In recent years, an aging population and rising obesity rates have contributed to higher incidence of
“This new payment model helps address a broken set of incentives that have prevented far too many Americans from benefiting from enjoying the better lives that could come with more convenient dialysis options or the possibility of a transplant,” said HHS Secretary Alex Azar, who said he had personally seen the effect of misaligned incentives when his own father battled kidney disease before he died in April.
ESRD, Azar said, remains one of the glaring examples in medicine where the US health care system pays more for patients to be sick than to get them well, “and we don’t have very good outcomes to show for it.”
Azar’s father received a living donor transplant that added years to his life, but the HHS secretary said the donor faced “bureaucratic rules and restrictions.”
In
Elements of the new model include:
- Payment changes involve both ESRD facilities and managing clinicians. CMS will apply adjustments to the per treatment base rate under the ESRD Prospective Payment System, while paying the monthly capitation payment to clinicians who are required to participate. The idea is to offer incentives to both parts of the system to work with Medicare beneficiaries and caregivers who are deciding whether to receive dialysis at a center or at home.
- The model promotes kidney transplants by expanding the eligibility criteria for living organ donors to receive financial assistance to allow them to take time off; lost wages, child care, and elder care can be covered. Among 61 countries who report to the US Renal Data System, the United States ranks 39th for kidney transplants per 1000 dialysis patients, and only 2.9% of ESRD patients receive a transplant before dialysis starts. CMS officials estimated the availability of donor kidneys will rise 20% by 2030.
During a briefing with reporters, CMS Administrator Seema Verma said patients who are on home dialysis or who can get an early transplant fare better than other ESRD patients.
CMS said the new model allows flexibility for education about kidney care options to be provided by professionals other than a nephrologist. In its fact sheet, CMS said it would “monitor for potential coercion, steering, and inappropriate referrals to the targeted modalities by model participants,” and measure the effect of the model on hospitalization and mortality. The model spells out notification and attribution requirements.
However, the coalition Kidney Care Partners (KCP) said that while CMS had addressed some issues, concerns remain. “While the Model would expand the Kidney Disease Education benefit, we know that early education before patients enter the dialysis facilities is essential to helping patients understand and adopt home dialysis modalities,” the group said in a statement. KCP said waivers under the new model “do not include dialysis facilities and their multi-disciplinary care teams,” which are covered in legislation,
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.