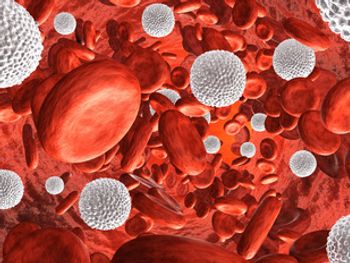
Neutropenia
Latest News
Latest Videos
CME Content
More News
Researchers have found that multiday corticosteroid administration during chemotherapy delays the diagnosis of and antimicrobial administration for febrile neutropenia.
Researchers have determined that febrile neutropenia has a low rate of bacteremia and approximately half of patients receive the recommended initial empiric therapy.
A study has demonstrated that D-index–guided early antifungal therapy, a novel approach to treating persistent or recurrent febrile neutropenia, is feasible in high-risk patients with neutropenia.
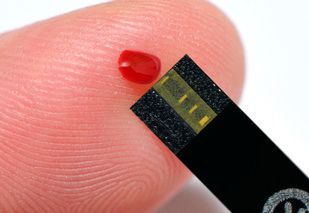
According to a study abstract presented at the 60th American Society of Hematology Annual Meeting & Exposition, using a skin patch for continuous temperature monitoring is feasible in the inpatient setting and has the potential to detect febrile neutropenia earlier.
In 2015, the Neulasta On-Body Injector (OBI) Onpro device was introduced as a less costly method of pegfilgrastim administration. While the device has been found to be safe in healthy volunteers and have pharmacokinetics similar to that of traditional pegfilgrastim, there have been limited data comparing the 2 methods.

Among older patients with non-Hodgkin lymphoma receiving myelosuppressive chemotherapy, use of primary prophylaxis with granulocyte colony-stimulating factor (G-CSF) increased significantly over the past 20 years.
Examining the frequency of bloodstream infection in these patients, researchers have found that staphylococcus aureus is most prevalent, followed by Klebsiella and E. coli.

Seeking to generate data for the development and validation of clinical decision rules in pediatric febrile neutropenia (FN), researchers used 2 decades of data on FN episodes in pediatric patients.
A single measurement of procalcitonin (PCT) is comparable to Multinational Association for Supportive Care in Cancer (MASCC) score for predicting serious medical complications in patients with cancer with febrile neutropenia.

More than 2 weeks of treatment with cefepime administered by intravenous (IV) push significantly increases the risk of cefepime-induced neutropenia.

Patients with neutropenia who have multidrug-resistant organisms have better rates of overall survival when receiving granulocyte transfusions within 7 days of neutropenic sepsis.

A new study comparing 2 risk stratification models found that the Clinical Index of Stable Febrile Neutropenia (CISNE) Model is useful for identifying low-risk patients with febrile neutropenia, but the combination of the CISNE Model with the Multinational Association of Supportive Care in Cancer Risk Index Score may help emergency physicians cope with febrile neutropenia more confidently.
Assessing the alternation of first-line antibiotics to avoid antibiotic resistance, researchers have determined that the strategy results in an increase in heterogeneity without increasing mortality.

Despite a meaningful survival, neutropenia is independently associated with poor outcomes among critically ill patients with cancer, according to a new study. However, neutropenia was no longer significantly associated with outcome in patients treated with granulocyte colony-stimulating factor (G-CSF), suggesting a beneficial impact of the treatment.
Incidence of febrile neutropenia, hospitalizations, and chemotherapy dose reductions and/or delays were similar between short- and long-acting granulocyte-colony stimulating factors, according to a meta-analysis of randomized controlled trials.

Pediatric patients with autoimmune neutropenia have a higher prevalence and cost than previously suspected, according to the results of 2 studies presented at the 60th American Society of Hematology Annual Meeting & Exposition, held December 1-4 in San Diego, California.

Among patients with pancreatic cancer being treated with modified FOLFIRINOX, those who develop severe neutropenia have significantly longer median overall survival, as well as longer time to treatment failure, compared with those who do not develop severe neutropenia.
New clinical guidelines are providing guidance for clinicians on the diagnosis, prevention, and treatment of febrile neutropenia in adult patients with solid tumors.
Patients who undergo outpatient autologous stem cell transplantations (ASCTs) not only report lower costs and higher satisfaction, but they also have lower odds of developing febrile neutropenia and septicemia than patients who undergo inpatient ASCT, according to the results of a new analysis.
Greater infection rate, higher white blood cell, monocyte, and absolute neutrophil counts are more significantly associated with severe congenital neutropenia than with patients with idiopathic and recovered neutropenia, according study results.
The quick sequential (sepsis-related) organ failure assessment can help emergency department physicians identify which patients with neutropenia are at risk of a poor prognosis and should receive prompt empirical antimicrobial therapy, according to a new study.
One-third of neutropenic patients developed invasive infection following intensive chemotherapy, which was significantly associated with an increase in mortality up to 100 days after the start of neutropenia.
Seeking to determine how FN is managed in most referral hospitals in Iran, researchers studied patients hospitalized during a 6-month period, also taking into account characteristics of FN patients and the risk factors associated with FN development.

Coverage of our peer-reviewed research and news reporting in the healthcare and mainstream press.
Adjusted incidence rate ratios showed that febrile neutropenia following chemotherapy carried an approximately 2-fold risk of long-term infection.