
Several evidence-based health literacy resources may be beneficial in health plan settings to improve organizational health literacy, personal health literacy, and health equity.

Several evidence-based health literacy resources may be beneficial in health plan settings to improve organizational health literacy, personal health literacy, and health equity.

Up to 257 million Americans could benefit from these prior authorization reforms that could have cross-market implications on health care plans administered through commercial insurers, Medicare Advantage, and Medicaid.

The top 5 podcasts for 2024 cover Medicare Advantage prior authorization, health equity, global immunization challenges, trauma-informed care, and health literacy.

Medicare Advantage beneficiaries with chronic obstructive pulmonary disease (COPD) who were invited to enroll in a program that reduced inhaler costs and provided medication management had higher inhaler adherence; however, there was no significant impact on exacerbations or overall health care spending.

As health care leaders, it’s our responsibility to know the importance of psychological safety and actively promote an environment that supports emotional and mental well-being, no matter one’s position or background, notes Carolyn Tandy of Humana.

For patients prescribed diabetes, hypertension, and hyperlipidemia medications, nonadherence to CMS Star Ratings quality measures of medication adherence was associated with increased health care resource utilization and costs.

As provider and payer organizations pursue the Quadruple Aim, it is important that they take into account not just the contracting but also the transformation in staffing, clinical workflows, and culture as these organizations evolve.

On this episode of Managed Care Cast, we're talking with the authors of a study published in the February 2024 issue of The American Journal of Managed Care® about their findings on how health plans can screen for health literacy, social determinants of health, and perceived health care discrimination.

Patients seen at value-based care clinics received more preventive screenings and had lower risks of hospitalization and emergency room visits, according to Humana’s 10th annual value-based care report.
At the Pharmacy Quality Alliance (PQA) 2023 Annual Meeting, the strategy advancement lead at Humana talked more about Humana’s health equity strategy and areas that pharmacy benefit managers (PBMs) and health plans can influence.

Over the next 18 to 24 months, Humana is exiting the commercial health plan business to focus on government-funded programs, like Medicare Advantage, and specialty businesses.

The first 5 minutes of a patient’s visit with a doctor can help improve communication and build more trusting relationships, explained panelists during a session on lung health disparities in America at CHEST 2022.

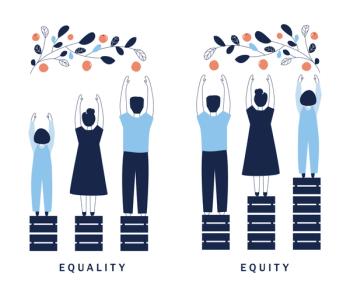
Humana developed a novel health disparities measure to guide disparity-focused initiatives and track progress in achieving health equity.

A large national survey of older adults enrolled in Medicare Advantage found a high collective burden of health-related social needs.

Geoffrey Boyce, CEO of Array Behavioral Care, explains how Array is responding to the increasing demand and utilization of mental health and behavioral services.

Panelists touted the ability to pay for items and repairs to keep Medicare beneficiaries healthier at home, avoiding potentially costly hospitalizations and complications.

Medicare advantage beneficiaries who received care from providers in 2-sided risk payment models had lower rates of acute care use, according to new study findings.

Geoffrey Boyce, CEO of Array Behavioral Care, explains how behavioral health care differs between in-person and telehealth care.

Geoffrey Boyce, CEO of Array Behavioral Care, discusses Array AtHome’s telebehavioral health services, which are now available to approximately 5 million Humana Medicare Advantage members.
Experts discuss current trends in Medicare Advantage during the current annual enrollment period, best practices for communication, and gain clarity about the benefits and costs for both providers and beneficiaries.

Experts discuss current trends in Medicare Advantage during the current annual enrollment period, best practices for communication, and gain clarity about the benefits and costs for both providers and beneficiaries.

Experts discuss current trends in Medicare Advantage during the current annual enrollment period, best practices for communication, and gain clarity about the benefits and costs for both providers and beneficiaries.

Experts discuss current trends in Medicare Advantage during the current annual enrollment period, best practices for communication, and gain clarity about the benefits and costs for both providers and beneficiaries.
Experts discuss current trends in Medicare Advantage during the current annual enrollment period, best practices for communication, and gain clarity about the benefits and costs for both providers and beneficiaries.
Experts discuss current trends in Medicare Advantage during the current annual enrollment period, best practices for communication, and gain clarity about the benefits and costs for both providers and beneficiaries.

Experts discuss current trends in Medicare Advantage during the current annual enrollment period, best practices for communication, and gain clarity about the benefits and costs for both providers and beneficiaries.

Experts discuss current trends in Medicare Advantage during the current annual enrollment period, best practices for communication, and gain clarity about the benefits and costs for both providers and beneficiaries.

On this episode of Managed Care Cast, we discuss senior health needs amid the pandemic and how Centerwell Senior Primary Care's holistic, team-based approach and value-based care delivery contributed to upticks in senior patient visits despite fears of COVID-19.

With the Oncology Care Model (OCM) slated to end in 2022, the successor model is still not in place. According to panelists, there is likely going to be a gap after OCM ends and the new model begins, but more importantly, practices should prepare for the new model to be mandatory.

Larger primary care practices in downside risk–only payment models and capitation saw the highest telemedicine utilization rates by their patients enrolled in Medicare Advantage (MA) plans.

259 Prospect Plains Rd, Bldg H
Cranbury, NJ 08512
© 2025 MJH Life Sciences®
All rights reserved.
