Payers
Latest News
Latest Videos

CME Content
More News

Addressing rural care is a way of addressing health inequities, and the Biden administration’s recent investment in rural care reflects its commitment to addressing health equity, said Ryan Urgo, MPAP, managing director, health policy, Avalere.
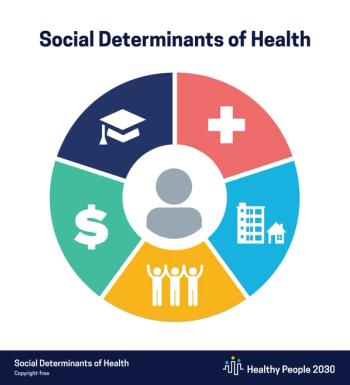
At the Pharmacy Quality Alliance (PQA) 2022 Annual Meeting Wednesday, participants heard about some unexpected insights arising from a workshop held this week between patients and pharmacists who are creating a patient-centered outcomes research agenda focused on addressing social determinants of health (SDOH) in the community pharmacy setting.

Adam Fein, PhD, of Drug Channels Institute, and Doug Long of IQVIA discussed trends in the specialty pharmacy market in the United States.

Representatives from employers, pharmacy benefit managers, and others discussed methods of improving pharmacy access and affordability in health plans.

Value-based payments were a benefit during the pandemic, but it remains to be seen if patients are interested in keeping those changes in care delivery as the pandemic recedes, said Jayson Slotnik, partner, Health Policy Strategies, Inc.
There are several pieces of legislation that could have an impact on drug rebates, explained Tracy Russell, senior director, government affairs, CoverMyMeds.
The approval of aducanumab (Aduhelm) was very controversial. There are 3 promising Alzheimer disease drugs in the pipeline with trials evaluating the efficacy, and there is a huge unmet need for these therapies, said Ray Tancredi, RPh, MBA, CSP, divisional vice president, specialty pharmacy development and brand Rx/vaccine purchasing, Walgreens.

Not only did a majority of each group say they hadn’t heard of biosimilars, but those who had heard of them had negative perceptions.
Patricia Deverka, MD, MS, senior researcher, deputy director at the Center for Translational and Policy Research and Precision Medicine, University of California San Francisco, explains what multicancer early detection tests currently exist and the research needed to understand their clinical utility.

The opening plenary of the Spring 2022 National Association of Accountable Care Organizations conference focused on addressing health equity and improving synergy between CMS and ACOs.

To achieve health equity, experts from CVS Health discuss why we must invest in programs that improve access to health care for historically marginalized communities, address social determinants, boost health education, increase representation in all levels of health care delivery, widen access to clinical trial research, and more.

Nathan H. Walcker, MBA, chief executive officer, Florida Cancer Specialists & Research Institute (FCSRI), discusses what guests can expect at the in-person Tampa meeting of The American Journal of Managed Care®'s Institute for Value-Based Medicine® (IVBM), co-hosted by FCSRI.

Increased uptake of biosimilars on par with the utilization rates of filgrastim biosimilars could have saved Medicare Part D $84 million in 2019.

Elaine Siegfried, MD, professor of pediatrics and dermatology, Saint Louis University Health Sciences Center, discusses several pediatric patient populations with atopic dermatitis who are candidates for the use of systemic therapies.

Key opinion leaders addressed cost, accessibility, and other barriers limiting use of comprehensive genomic profiling (CGP), and how employers can help drive preventive care and precision medicine through CGP.

Joseph Alvarnas, MD, vice president of government affairs at City of Hope and chief clinical adviser of AccessHope in Duarte, California, spoke March 4 at the closing session of the Association for Community Cancer Centers (ACCC) Annual Meeting & Cancer Business Summit in Washington, DC.

Predictive models can help find high-risk patients with asthma and manage them proactively, but prior models miss the highest-risk patients and may mislabel low-risk patients.

Alymsys from Amneal Pharmaceuticals and mAbxience is the third biosimilar referencing Avastin approved in the United States and the second of 3 biosimilar approvals Amneal expects in 2022.


Delayed diagnosis of wild-type transthyretin amyloid cardiomyopathy (ATTR-CM) results in inappropriate treatments prior to diagnosis and worse clinical outcomes after diagnosis.

News on 2 new CAR T-cell therapies and updates on PARP inhibitors, BTK inhibitors, and biosimilars.
Coverage from the Community Oncology Alliance 2022 Community Oncology Conference, held March 17-18 in Kissimmee, Florida.

Across OneOncology, says Edward Arrowsmith MD, MPH, clinical pathways offer a vehicle for physicians to agree on best practices and to implement them across the network. Early this year, Arrowsmith became medical director for Clinical Pathways, OneOncology.

In Medicaid, delivering care needs to address the lack of resources and other socioeconomic factors that impact patients, said Steve Evans, MD, chief medical officer of SilverSummit at Centene.

More than a quarter of patients experience disruptions and delays in treatment for chronic heart failure (CHF) after the initial prescription for sacubitril/valsartan was abandoned/rejected.