- October 2021
- Volume 27
- Issue 7
Conversations on CAR T: Study of Checkpoint Inhibitors After Transplant Bolsters Case for CAR T, Skarbnik Says
The second of Evidence-Based Oncology™’s summer interviews with experts on diffuse large B-cell lymphoma (DLBCL) is with Alan Skarbnik, MD, director of the Lymphoma and Chronic Lymphocytic Leukemia (CLL) program and director of the Experimental Therapeutic and Immune Effector Cell Program at Novant Health Cancer Institute in Charlotte, North Carolina.
In May, Skarbnik was lead author of an article on phase 1b results on safety and clinical effects of combining checkpoint inhibition therapy (ipilimumab and nivolumab) after autologous stem cell transplant (ASCT)1 for patients with high-risk DLBCL, mature T-cell lymphoma, and multiple myeloma. Although the cohorts were small and Skarbnik describes the findings as “hypothesis driving,” progression-free survival (PFS) and overall survival (OS) at 18 months post-ASCT were highest in the primary refractory DLBCL cohorts, at 85% and 100%, respectively. In relapsed DLBCL, the results were not as promising: PFS was 28.6% and OS was 57.1%.1
As Skarbnik explains, the phase 1b study (NCT02681302) was planned before the first chimeric antigen receptor (CAR) T-cell therapies were approved—but it informs the bottom line being reported today: immunotherapy approaches in primary refractory DLBCL may be superior to cytotoxic chemotherapy with transplant.
This interview has been edited for length and clarity.
EBO: In May, you published results involving the use of combined checkpoint inhibitors following ASCT in DLBCL and other conditions. Can you discuss the overall findings?
SKARBNIK: The study first [sought] to evaluate the safety of this approach, using combined checkpoint inhibitors, nivolumab and ipilimumab, immediately following autologous stem cell transplantation. That combination had not been used before in that specific setting, and we wanted to evaluate whether it was safe and feasible The second end point investigated outcomes, particularly in terms of PFS and OS. For patients with high-risk, multiple hematologic malignancies, there were different cohorts. We had 1 cohort for patients with primary refractory DLBCL and a cohort for patients who had early relapse DLBCL within the first year after frontline treatment.
We had 2 cohorts for T-cell lymphoma: 1 for advanced stage frontline consolidation, the other for relapse or refractory peripheral T-cell lymphoma. We excluded ALK-positive anaplastic large cell lymphoma from this cohort because we know they have better outcomes. Then we had 2 myeloma cohorts: 1 for high-risk multiple myeloma by cytogenetics as frontline consolidation and the other for myeloma that relapsed within 3 years of an up-front transplant—so [this would] be a second transplant with the checkpoint inhibitor consolidation.
In this study, we did not identify any new safety signals, when compared with previous studies—these drugs are largely used in solid tumors—for lung, for renal cancer and melanoma. The adverse effects [AEs] were largely immune-related and were treated with steroids. We saw more cytopenias with these agents than in other settings, but cytopenias are very common following transplantation, so there’s a confounding factor.
EBO: What about efficacy in DLBCL? What differences did you observe?
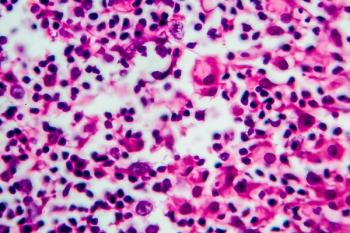
SKARBNIK: Efficacy seems to be largely dependent on the disease state we used it for; this is a phase 1 study, and is mainly hypothesis driving. Cohorts had small numbers; each cohort had 7 patients, except for the T-cell cohorts, that were closed early due to slow accrual. The cohort of primary refractory DLBCL had 7 patients. Most of them were not in complete remission after 2nd line therapy before undergoing transplant. Patients were allowed enrollment in the trial with active disease as long as there was no progression through the previous line of salvage therapy. We allowed for stable disease or partial responses to the most recent salvage therapy. Most of the patients had a partial response in that cohort, and all the patients presented with complete response after transplant and checkpoint inhibitor consolidation.
Of the 7 patients, only 1 patient presented progression of disease in a small lymph node. The patient was treated with radiation therapy and rituximab, entered remission again and is still in remission. All other patients remain progression and disease free, and it’s been over 3 years of follow-up.
This is a disease state where the median overall survival after transplant is close to 14 months. Again, it’s hard to compare different trials, particularly in a very small population. But it raises a question: Is it a reasonable and efficacious approach? It will take a larger trial to confirm that.
However, in the cohort of patients with DLBCL that achieved a complete remission and then presented relapse within the first year—which was the second cohort of DLBCL—we didn’t see similar outcomes. At 18 months, the PFS was 28.6% and OS was 57%. So there’s a potentially different efficacy signal there. We’re not sure why that happened. It could be because there were small numbers and this difference is random. It could be that there are actual biological differences in the disease states. What we tried to accomplish with this approach was to skew the post-transplant immune reconstitution toward an effector phenotype rather than a tolerance phenotype, by using checkpoint inhibitors.
Usually, after autologous stem cell transplantation the first immune cells to recover are regulatory T cells, which may hinder an effective immune response against cancer. By using this combination, we tried to flip that and increase the T effector component to allow for an anti-cancer immunologic effect. We observed differences in the immunologic profiles between the two DLBCL cohorts, using this approach. In the primary refractory DLBCL cohort, the regulatory T-cells remained low for 18 weeks following transplantation, with a corresponding early increase in the effector T-cell population.
In the early-relapsed DLBCL cohort, there was no significant decrease in the regulatory T-cell component and the effector T-cells remained low until 12 weeks post transplant. These differences may explain the contrasting outcomes between those two cohorts.
EBO: Even if it’s small numbers, though, you’ve simultaneously addressed all the big issues that come up in DLBCL. Patients relapse—and what is the right therapy once the relapse happens? What’s the right sequence when there are so many choices? Once there is a transplant, what comes next? You’ve looked at a lot of those challenges.
SHARBNIK: Yes, we did. Let me remind you that when the study was written and started, CAR T cells weren’t approved. We started writing the study in 2015, and the study started in 2016 before the commercial approval of CAR T cells.
I think what’s clear to the lymphoma community is that for patients who present primary refractory disease and/or early relapse of disease—especially within the first 6 to 12 months following frontline therapy—chemotherapy is not the answer. The disease has shown its face and it doesn’t generally respond to more chemotherapy. It’s different than a disease that comes 2 years later or even more than a year later, where you do have still a chance to salvage those patients and then consolidate with autologous stem cell transplantation. We know that stem cell transplantation on its own is basically very high-dose chemotherapy—the stem cell transplant is a rescue for the myelotoxicity that the chemotherapy causes. There’s a minimal immunologic effect for a very short period after recovery, but that’s it.
We’ve seen with the CAR T experience—there have been press releases, but we don’t have all the data yet—that in 2 trials [NCT03391466; NCT03575351] comparing chemotherapy and transplant vs CAR T2,3 in the second-line setting for patients with primary refractory [and] early relapse disease [that] there’s superiority in terms of event-free survival in [the CAR T] patients.
The experience in the past show that it’s very hard to treat primary refractory DLBCL. The option we had before was to take the patient to transplant with potential residual disease after salvage, and those are the patients who generally end up presenting a relapse. So, the idea of the [phase 1] trial was to shift that perspective and include some immunotherapy in the fold to improve on efficacy. It is a different process, but to some extent it is the same idea behind CAR T-cell therapy—using an immunologic approach rather than a purely cytotoxic chemotherapy approach.
As of today, we don’t yet know what’s the ideal process for treating these patients. Fortunately, we have more options coming on board. There are bispecific antibodies that are being studied for DLBCL; I think they are going to have a very strong place in the treatment of patients with refractory or early relapse disease. We need to go beyond cytotoxic chemotherapy for primary refractory disease, and evaluate immunotherapy beyond rituximab.
EBO: In terms of the approach [in this study], you’ve ried some of the more standard immunotherapy—we’ve had CAR T come online, we’ve had [tafasitamab] come online. Would you try these therapies?
SKARBNIK: I’m a big fan of CAR T cells. I think CAR T cells in the second-line setting may be very reasonable; there’s a good rationale for that but we need to wait for the complete dataset from the studies comparing CAR T with autologous stem cell transplant in second line to draw conclusions. It seems that the earlier you use these therapies, when you have less T cell exhaustion, they may be more effective in driving responses. Once patients have seen 3 or 4 lines of chemotherapy, T cells are likely to be more exhausted.
In terms of logistics, CAR T cell therapy is certainly easier than this approach that we studied. First, there’s the transplant and then there are almost 6 months of consolidation with immunotherapy using an intensive schedule.
There are new agents coming on board. Tafasitamab is approved; we have loncastuximab tesirine approved, which is an antibody-drug conjugate that also targets CD19. We do have CAR T, which is likely to come to second line in the very near future, and have the bispecific [antibodies], with ongoing studies for DLBCL. Again, I think the point to make is that an immunologic approach for primary refractory or early relapsed DLBCL seems more promising than the traditional cytotoxic
chemotherapy approach with stem cell transplant.
References
1. Skarbnik AP, Donato ML, Feinman R, et al. Safety and efficacy of consolidation therapy with ipilimumab plus nivolumab after autologous stem cell transplantation. Transplant Cell Ther. 2021;27(5):391-403. doi:10.1016/j.jtct.2020.12.026.
2. Kite announces Yescarta CAR T-cell therapy improved event-free survival by 60% over chemotherapy plus stem cell transplant in second-line relapsed or refractory large B-cell lymphoma. News release. Gilead. June 28, 2021. Accessed September 16, 2021. https://bit.ly/3zbZOSU
3. Bristol Myers Squibb announces positive topline results from phase 3 TRANSFORM trial evaluating Breyanzi (lisocabtagene maraleucel) versus chemotherapy followed by stem cell transplant in second-line relapsed or refractory large B-cell lymphoma. News release.
Bristol Myers Squibb. June 10, 2021. Accessed September 16, 2021. https://bit.ly/2VPLvWA
Articles in this issue
over 4 years ago
From the Editor-in-Chief: The Way Upover 4 years ago
Building a Patient-Centered Cancer Center From the Ground Upover 4 years ago
The Promise of Liquid Biopsies for Cancer DiagnosisNewsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.