- October 2023
- Volume 29
- Issue 8
- Pages: SP654-SP657
COVID-19 Fallout on Individuals, Economy, and Health System to Last for Years, White Paper Concludes
The federal government may have declared an end to the public health emergency for COVID-19 on May 11, 2023,1 but the effects of this infectious disease that caused nearly 7 million confirmed deaths worldwide by October 20232 will not end for the US health care system anytime soon.
In fact, the effects of long COVID will exact both a public health and economic toll for years to come, according to a white paper developed in the summer of 2023.3
The white paper was produced following the Long COVID, Inflammation, and Cancer Conclave held May 11-12, 2023, in Charlotte, North Carolina, to bring together global researchers, health care experts, and philanthropists interested in understanding the long-term effects of COVID-19 across the health system.4 The event was presented by No One Left Alone and chaired by Kashyap Patel, MD, immediate past president of the Community Oncology Alliance and CEO of Carolina Blood and Cancer Care Associates, and Afshin Beheshti, MD, president of the COVID-19 International Research Team and bioinformatician and principal investigator at NASA Ames Research Center.
The topics covered a range of issues around long COVID, also known as postacute sequelae of COVID-19 (PASC).5 Some speakers focused on identifying links between long COVID, microRNA, inflammation, and therapeutic interventions; others discussed COVID-specific microRNA detection, mitochondrial function in SARS-CoV-2 and cancer, methylation metrics, real-world data from community practice, and more, aiming to understand the long-term consequences of COVID-19 and its connection to cancer and other health conditions.
According to Patel, despite the COVID-19 public health emergency being lifted as the meeting began,1 there are still tens of millions of Americans dealing with long COVID—and perhaps close to 100 million globally.6
“Given the vast number of individuals infected by this virus, the magnitude of this health crisis from individual health to human suffering and overall impact on global population health and economies—including direct spending on health care issues resulting from long COVID and indirect expense from lost work, mental health crisis, and global economy—is easily recognizable,” Patel said in a call to action that concluded the meeting.
How Does Long COVID Affect the Body?
Long COVID or PASC is a complex, multi-organ illness that arises in individuals with a history of SARS-CoV-2 infection, typically emerging around 3 months after the onset of COVID-19 symptoms. These symptoms—which can last for months or years—cannot be attributed to another diagnosis and are often connected to ongoing inflammatory changes in multiple tissues. PASC affects up to 80% of individuals who have had COVID-19,7 with between 2.5% and 15% experiencing more prolonged symptoms.8 Notably, fatigue is the most frequently reported symptom, yet it is also a symptom for several other conditions, making it harder to pinpoint the cause.
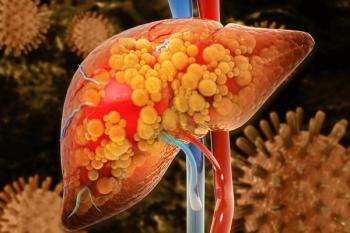
Additionally, more severe cases of long COVID can lead to damage in various organ systems such as the lungs, heart, nervous system, kidneys, and liver, alongside conditions like thrombotic and cerebrovascular diseases, type 2 diabetes, and mental health impairments.9
Long COVID also intersects with cardiovascular disease (CVD) and patients with both conditions can display persistent symptoms such as dyspnea, fatigue, chest pain, and cough. Around 20% of patients continue to experience these symptoms 3 months after initial COVID-19 infection. As discussed during the conclave, the occurrence of COVID-19–associated myocarditis is estimated at 150 cases per 100,000 individuals, often resulting from multiple contributing factors.10 Chest pain remains a common CVD symptom for individuals with moderate to severe COVID-19 infection, with myocarditis and pulmonary embolism presenting as higher risks for these individuals compared with other CVD complications. Data from the US Department of Veterans Affairs database suggest there is an increased risk of heart failure, dysrhythmias, and stroke 1 year after SARS-CoV-2 infection.11
Neurological complications are also prevalent in long COVID, impacting up to a third of patients.12 These complications can affect either the central or peripheral nervous system and include fatigue, cognitive impairment, headache, mood disorders, smell and taste disorders, and sensorimotor deficits. Cognitive dysfunction caused by long COVID also influences attention, executive function, problem-solving, and decision-making, with memory impairment seen in many cases, even among younger individuals.13
Brain imaging studies have also revealed consistent changes across various brain areas, including the temporal lobe, hypothalamus, brain stem, and cerebellum.14 According to speakers at the conclave, COVID-19 infection may pose a risk for the development of neurodegenerative diseases, dementia, and mild cognitive impairments, even in relatively young adults.
Other significant health issues linked to long COVID include persistent cognitive and mental health disorders, muscle and joint pain, fatigue, inflammation, and multi-organ damage. Research suggests that approximately 70% of patients with long COVID experience damage to at least 1 organ, while studies on renal functions in veterans with COVID-19 indicate increased kidney damage risk.15
How Does Long COVID Affect Population Health?
It’s estimated that—based on a conservative estimate of 10% of individuals with COVID-19 developing more prolonged PASC—more than 65 million people globally are affected by long COVID.9 In the United States alone, more than 27 million people are presumed to have been affected by long COVID by spring 2023.16 PASC is prevalent across age groups and levels of disease severity, with most diagnoses occurring in patients aged between 36 and 50 years and a significant proportion of cases involving nonhospitalized patients with mild acute illness.9
What Is the Economic Impact of Long COVID?
The projected economic impact of long COVID is estimated to be around $3.7 trillion—more than $1 trillion over initial estimates made in 2020—with direct and indirect costs ranging from $140 billion to $600 billion annually.17 Nearly 60% of these costs are due to reduced quality of life, with the remainder due to reduced earnings and greater medical spending. This translates to about $11,000 per person.
As of August 2022, about 16 million working-age Americans aged 18 to 65 years were reported to have long COVID.18 Of this group, around 4 million were unable to work because of the condition, resulting in about $170 billion in lost wages.
PASC exerts an even bigger strain on the health care system, contributing to a yearly financial burden of nearly $400 billion in the United States, and is expected to remain one of the top 10 medical cost drivers for the next 5 years. As research has shown the neurological symptoms of long COVID, its impact on functional ability and workplace productivity is substantial. This has been seen particularly in cases of myalgic encephalomyelitis from long COVID, in which the persistence of neurocognitive symptoms led to estimated annual costs of $9000 per patient.17,19
Looking at both the workplace and the health care setting, long COVID can lead to a reduction in work hours for 46% of patients and a $6200 increase in annual emergency department visits and possibly more than 20 outpatient visits within a year.20
Does Long COVID Exacerbate Existing Disparities?
The short answer? Yes.
The longer answer? COVID-19 exacerbated existing inequalities among marginalized communities. This has led to a range of issues such as delayed diagnoses, reduced health care accessibility primarily driven by inadequate health insurance coverage in Black and Latinx populations, postponed or absent medical treatment, and heightened vulnerability to SARS-CoV-2 exposure, and that was only in the first year of the pandemic.21
Since then, research supported by the National Institutes of Health RECOVER program has uncovered disparities in the impact of long COVID symptoms across racial and ethnic groups in the United States, specifically among Black and Hispanic patients.22 It was found that Black and Hispanic Americans tend to experience a higher burden of symptoms and health issues related to long COVID compared with White patients.
In the study, racial and ethnic minority groups demonstrated significantly higher adjusted odds of being diagnosed with various symptoms and conditions affecting multiple organ systems compared with White patients. Notably, among nonhospitalized patients with COVID-19, Hispanic individuals had higher odds of long COVID diagnosed in 6 organ systems, while Black individuals had higher odds in 4 organ systems.
Among hospitalized patients, the disparities were even more pronounced, particularly when looking at patients’ endocrine and circulatory systems. For example, compared with White patients, Black patients were twice as likely to develop diabetes and 1.5 times more likely to experience chest pain within 30 to 180 days after infection. Similar disparities were observed among Hispanic individuals.22
According to researchers who conducted a cohort study from the RECOVER program, these disparities are likely influenced by a complex interplay of biological, environmental, and social factors, including variations in immunogenetics that affect immune profiles and cytokine levels.23 These findings underscore the importance of understanding and addressing the underlying reasons for these disparities in long COVID outcomes among different racial and ethnic groups.
What is the Link Between Long COVID and Cancer?
The connection between viral infections and cancer risk, dating back to the discovery of virus-associated lymphoma in 1964,24 underscores that around 15% to 20% of cancer cases stem from carcinogenic infections, primarily viral.25 At least 7 human oncogenic viruses—including Epstein-Barr virus, human papillomavirus, and hepatitis B and C viruses—are closely linked to various human cancers. Mechanisms contributing to this process are diverse, and include chronic inflammation, immune suppression, alterations in DNA modification, mitochondrial function, and activation of oncogenes and tumor suppressors. Additionally, tumorigenesis is linked to chronic inflammation and persistent infections, with viruses needing immune evasion mechanisms and infections inducing mild but lasting inflammation.26 Chronic inflammation also heightens mutation rates, elevating cancer risk.
Long COVID is characterized by inflammatory pathway activation, demonstrated by an early, intense inflammatory response alongside reduced anti-inflammatory activity and mitochondrial stress. Neutrophil dysfunction in even mild cases could heighten cancer susceptibility because of low-density neutrophil (LDN) increase, known for immunosuppression.27 The rise in LDNs correlates with poor T-cell response and disease severity, suggesting potential control limitations and altered neutrophil-to-lymphocyte ratio.
The lasting effects of residual virus cells may induce chronic inflammation and oxidative stress, leading to tissue and DNA damage.26 The spike protein of SARS-CoV-2 activates inflammasome and inflammatory pathways, particularly in older individuals, possibly contributing to age-related comorbidities and immune response impairment. This, coupled with immune evasion strategies of the virus, suggests long COVID’s potential as a risk factor for new cancer through various mechanisms, including chronic virus infection, inflammation, cell senescence, the oncogenic potential of SARS-CoV-2, and immunosuppression.
At the cellular level, the pathophysiology of long COVID involves immune imbalances, incomplete viral clearance, and potentially mitochondrial dysfunction.28 Recent evidence has also highlighted the virus’ targeting of mitochondria, disrupting their function. This occurs through virus-encoded proteins such as ORF-96 and ORF-3a, which alter mitochondrial genes and homeostasis, ultimately leading to apoptosis and the release of mitochondrial DNA. The degraded mitochondrial DNA, found at high levels in the blood, can predict poor COVID-19 outcomes. In individuals with compromised mitochondrial function, the virus might induce chronic inflammation and metabolic imbalance, driving long COVID symptoms. This state is characterized by mitochondrial dysfunction, ongoing inflammation, and a shift toward glycolysis. Restoring metabolic balance through interventions such as physical activity or with compounds that enhance mitochondrial function could be beneficial.
A New Way to Detect COVID-19?
MicroRNAs (miRNAs) are small non-coding RNAs with crucial roles in post-transcriptional gene regulation, and they have a significant impact on diseases such antiviral responses.29 A particular circulating miRNA, miR-2392, is linked to SARS-CoV-2 machinery when the host is infected. It contributes to suppressing mitochondrial gene expression, increasing inflammation, glycolysis, hypoxia, and COVID-19–associated symptoms. Additionally, miR-2392 is detected in blood and urine of patients with COVID-19, suggesting its potential use for minimally invasive COVID-19 detection. A miRNA-based antiviral therapeutic targeting miR-2392 reduces SARS-CoV-2 viability in hamsters, offering a potential avenue to mitigate COVID-19 infection in humans.
The immunological profiles of individuals with long COVID differ from those who recover quickly, with patients with long COVID showing a decrease in interferon gamma (IFN-γ) producing CD8+ cells 4 months after symptom onset.30 Cytotoxic lymphocytes, which impact viral clearance through IFN-γ release, seem affected. DNA methylation is a stable epigenetic marker with significant roles in normal biological processes and disease pathogenesis.31 Genomic and epigenetic studies have unveiled susceptibility genes for COVID-19, particularly ACE2, and demonstrated that methylation patterns can predict disease severity.32 Understanding the connection between epigenetic variation and infection involves analyzing how hosts respond to viral exposure, how viruses utilize the host’s epigenome to establish infection, and the inherent susceptibility differences between individuals.
When Will Biomarker Testing Be Available?
Since the spring, Evidence-Based Oncology has contacted multiple payer organizations—some more than once—seeking comment on the impact of long COVID and the potential availability of biomarker testing, following publication of Patel’s initial call to action on March 22.33 Patel’s comments appeared 2 months after a review article on long COVID, led by senior author Eric J. Topol, MD, concluded that “Diagnostic and treatment options are currently insufficient, and many clinical trials are urgently needed to rigorously test treatments that address hypothesized underlying biological mechanisms, including viral persistence, neuroinflammation, excessive blood clotting and autoimmunity.”9
Payer organizations contacted include Blue Cross and Blue Shield of Louisiana, Horizon Blue Cross Blue Shield of New Jersey, Anthem Blue Cross Blue Shield Indiana and Anthem Blue Cross Blue Shield New York, Centene, Humana, EmblemHealth, Priority Health, and Highmark. These organizations either did not respond to email or declined to comment.
“The lack of biomarker testing makes the disparities worse, and I think payers have an obligation to [put] some sort of process in place so that they can at least do their part of the work in addressing disparities,” Patel said. “By not saying what they plan to do is tantamount to denying patients the appropriate treatment options that are available based on scientific evidence.”
In discussing the lack of payer comment on biomarker testing for long COVID, Patel referenced the American Association for Cancer Research (AACR) Cancer Disparities Progress Report 2020, which highlights an urgent need for implementing guideline-concordant biomarker testing to reduce costs, improve patient outcomes, and address health care disparities.34
“I’m not surprised at the payers’ approach, but that’s the problem our country has,” Patel said. “It has itself a compartmentalized, fragmented system where the lobbyists let payers get away with whatever they want to get away with. This [AACR] article itself would undeniably mandate an inclusive approach,” Patel said.
According to Patel, it is imperative to shift our focus toward fact-based evidence generation, data collection, provider and payer education, intervention design, mass public education campaigns, and policy implementation. Although the exact pathophysiology of long COVID remains unclear, links have emerged among inflammation, altered immune responses, and long COVID manifestations. A proposed call to action that emerged from the conclave35 encompassed several aspects, such as:
- assessing the population health impact of long COVID and its relationship with cancer;
- evaluating the health care costs associated with long COVID and cancer;
- exploring the chronic comorbidities linked to long COVID;
- analyzing trends in new cancer cases among community cancer patients both pre- and post COVID;
- investigating the postpandemic ramifications on industry and payers resulting from long COVID;
- exploring the potential utility of the SARS-CoV-2 full spike protein as a biomarker for long COVID;
- uncovering the impact of COVID-19 infections on the epigenome of relevant tissues or blood and the development of epigenetic markers; and
- creating patient-derived organoid models from relevant tissues to better understand tumorigenesis.
Addressing these questions, Patel said, will provide insights into differences between vaccinated and unvaccinated patients, potential associations between long COVID and the emergence of rare cancers, the influence of biological factors on long COVID susceptibility, the persistence of SARS-CoV-2 in organs, the influence of host genetics and the microbiome, the potential for stage migration in cancer due to inflammation, the impact of severe inflammation on chronic end-organ damage, the establishment of common diagnostic criteria for long COVID, and the development of preventive and therapeutic strategies.
He also emphasized the need to explore strategies to prevent the reactivation of herpes family or other viruses due to COVID-induced immune dysfunction. To execute this call to action effectively, Patel proposed dividing it into 3 main themes, as follows:
- education, which includes educating health care providers, patients, payers, pharmaceutical companies, and the general public through awareness campaigns;
- research, which involves establishing a prospective real-world evidence registry for long COVID, identifying susceptibility factors, examining differences between vaccinated and nonvaccinated individuals, and investigating distinctions between patients with and without cancer; and
- intervention, with this category encompassing the development and implementation of therapeutic and health interventions as well as the provision of human services, support, and interventions.
For therapeutic interventions, Patel noted that research can include exploring anti-inflammatory approaches such as tumor necrosis factor-α inhibitors such as infliximab, kinase inhibitors such as imatinib, Janus kinase 2 inhibitors, Bruton tyrosine kinase inhibitors, anti-interleukin-6 treatments, and COVID-19–specific cytotoxic T lymphocytes for the treatment of acute-risk patients with COVID-19.
This comprehensive approach aims to address the multifaceted challenges posed by long COVID and provides a clear path forward for research, education, and intervention in response to this ongoing global health concern.
Mary Caffrey contributed to this report.
References
1. End of the federal COVID-19 public health emergency (PHE)
declaration. CDC. Updated September 12, 2023. Accessed
September 22, 2023. https://www.cdc.gov/coronavirus/2019-ncov/your-health/end-of-phe.html
2. WHO coronavirus (COVID-19) dashboard. World Health Organization. Updated September 27, 2023. Accessed October 2, 2023. https://covid19.who.int/
3. Patel K, Beheshti A. Exploring the interconnectedness of long COVID, inflammation, cardiovascular diseases, neurological issues, autoimmune disorder, psychological issues, and cancer: implications for population health and healthcare disparities. Presented at: Long COVID and Cancer Conclave; May 12, 2023; Accessed via June 19, 2023. Charlotte, NC.
4. Long COVID and Cancer Conclave Meeting. COVID International Research Team. May 12, 2023. Accessed October 2, 2023. https://www.cov-irt.org/long-covid-and-cancer-conclave-meeting-on-may-12th/
5. Long COVID. Yale Medicine. Accessed September 22, 2023. https://www.yalemedicine.org/conditions/long-covid-post-acute-sequelae-of-sars-cov-2-infection-pasc
6. Perumal R, Shunmugam L, Naidoo K. Long COVID: an approach to clinical assessment and management in primary care. S Afr Fam Pract (2004). 2023;65(1):e1-e10. doi:10.4102/safp.v65i1.5751
7. Landry M, Bornstein S, Nagaraj N, et al. Postacute sequelae of SARS-CoV-2 in university setting. Emerg Infect Dis. 2023;29(3):519-527. doi:10.3201/eid2903.221522
8. Whitaker M, Elliott J, Chadeau-Hyam M, et al. Persistent COVID-19 symptoms in a community study of 606,434 people in England. Nat Commun. 2022;13(1):1957. doi:10.1038/s41467-022-29521-z
9. Davis HE, McCorkell L, Vogel JM, Topol EJ. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. 2023;21(3):133-146. doi:10.1038/s41579-022-00846-2
10. Boehmer TK, Kompaniyets L, Lavery AM, et al. Association between COVID-19 and myocarditis using hospital-based administrative data – United States, March 2020-January 2021. MMWR Morb Mortal Wkly Rep. 2021;70(35):1228-1232. doi:10.15585/mmwr.mm7035e5
11. Abbasi J. The COVID heart-one year after SARS-CoV-2 infection, patients have an array of increased cardiovascular risks. JAMA. 2022;327(12):1113-1114. doi:10.1001/jama.2022.2411
12. Priyal, Sehgal V, Kapila S, Taneja R, Mehmi P, Gulati N. Review of neurological manifestations of SARS-CoV-2. Cureus. 2023;15(4):e38194. doi:10.7759/cureus.38194
13. Nehme M, Braillard O, Chappuis F; CoviCare Study Team; Guessous I. The chronification of post-COVID condition associated with neurocognitive symptoms, functional impairment and increased healthcare utilization. Sci Rep. 2022;12(1):14505. doi:10.1038/s41598-022-18673-z
14. Douaud G, Lee S, Alfaro-Almagro F, et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. 2022;604(7907):697-707. doi:10.1038/s41586-022-04569-5
15. Dennis A, Wamil M, Alberts J, et al. Multiorgan impairment in low-risk individuals with post-COVID-19 syndrome: a prospective, community-based study. BMJ Open. 2021;11(3):e048391. doi:10.1136/bmjopen-2020-048391
16. Packard SE, Susser E. Association of long COVID with housing insecurity in the United States, 2022-2023. medRxiv. June 19, 2023. 2023;2023.06.05.23290930. doi:10.1101/2023.06.05.23290930
17. Cutler DM. The economic cost of long COVID: an update. Harvard Kennedy School. July 16, 2022. Accessed October 2, 2023. https://www.hks.harvard.edu/centers/mrcbg/programs/growthpolicy/economic-cost-long-covid-update-david-cutler
18. Bach K. New data shows long Covid is keeping as many as 4 million people out of work Brookings. August 24, 2022. Accessed September 22, 2023. https://www.brookings.edu/articles/new-data-shows-long-covid-is-keeping-as-many-as-4-million-people-out-of-work/
19. Jason LA. Mirin AA. Updating the National Academy of Medicine ME/CFS prevalence and economic impact figures to account for population growth and inflation. Fatigue: Biomed. January 18, 2021. Accessed September 22, 2023. doi:10.1080/21641846.2021.1878716
20. Office of the Assistant Secretary for Planning and Evaluation. Impact of the COVID-19 pandemic on the hospital and outpatient clinician workforce: challenges and policy responses. US Department of Health and Human Services. May 3, 2022. Accessed October 2, 2023. https://aspe.hhs.gov/reports/covid-19-health-care-workforce
21. Ala A, Wilder J, Jonassaint NL, et al. COVID-19 and the uncovering of health care disparities in the United States, United Kingdom and Canada: call to action. Hepatol Commun. 2021;5(10):1791-1800. doi:10.1002/hep4.1790
22. Khullar D, Zhang Y, Zang C, et al. Racial/ethnic disparities in post-acute sequelae of SARS-CoV-2 infection in New York: an EHR-based cohort study from the RECOVER program. J Gen Intern Med. 2023;38(5):1127-1136. doi:10.1007/s11606-022-07997-1
23. Saini G, Swahn MH, Aneja R. Disentangling the coronavirus disease 2019 health disparities in African Americans: biological, environmental, and social factors. Open Forum Infect Dis. 2021;8(3):ofab064. doi:10.1093/ofid/ofab064
24. Epstein MA, Achong BG, Barr YM. Virus particles in cultured lymphoblasts from Burkitt’s lymphoma. Lancet. 1964;1(7335):702-703. doi:10.1016/s0140-6736(64)91524-7
25. Plummer M, de Martel C, Vignat J, Ferlay J, Bray F, Franceschi S. Global burden of cancers attributable to infections in 2012: a synthetic analysis. Lancet Glob Health. 2016;4(9):e609-e616. doi:10.1016/S2214-109X(16)30143-7
26. Amiama-Roig A, Pérez-Martínez L, Rodríguez Ledo P, Verdugo-Sivianes EM, Blanco JR. Should we expect an increase in the number of cancer cases in people with long COVID?. Microorganisms. 2023;11(3):713. doi:10.3390/microorganisms11030713
27. Siemińska I, Węglarczyk K, Surmiak M, et al. Mild and asymptomatic COVID-19 convalescents present long-term endotype of immunosuppression associated with neutrophil subsets possessing regulatory functions. Front Immunol. 2021;12:748097. doi:10.3389/fimmu.2021.748097
28. Blanco-Melo D, Nilsson-Payant BE, Liu WC, et al. Imbalanced host response to SARS-CoV-2 drives development of COVID-19. Cell. 2020;181(5):1036-1045.e9. doi:10.1016/j.cell.2020.04.026
29. McDonald JT, Enguita FJ, Taylor D, et al. Role of miR-2392 in driving SARS-CoV-2 infection. Cell Rep. 2021;37(3):109839. doi:10.1016/j.celrep.2021.109839
30. Lee Y, Riskedal E, Kalleberg KT, et al. EWAS of post-COVID-19 patients shows methylation differences in the immune-response associated gene, IFI44L, three months after COVID-19 infection. Sci Rep. 2022;12(1):11478. doi:10.1038/s41598-022-15467-1
31. Balnis J, Madrid A, Hogan KJ, et al. Blood DNA methylation and COVID-19 outcomes. Clin Epigenetics. 2021;13(1):118. doi:10.1186/s13148-021-01102-9
32. Corley MJ, Pang APS, Dody K, et al. Genome-wide DNA methylation profiling of peripheral blood reveals an epigenetic signature associated with severe COVID-19. J Leukoc Biol. 2021;110(1):21-26. doi:10.1002/JLB.5HI0720-466R
33. Klein H. Kashyap Patel, MD, sees link between COVID-19 and cancer progression, calls for more biomarker testing. Am J Manag Care. 2023;29(SP4):SP333-SP334.
34. Sengupta R, Honey K. AACR cancer disparities progress report 2020: achieving the bold vision of health equity for racial and ethnic minorities and other underserved populations. Cancer Epidemiol Biomarkers Prev. 2020;29(10):1843. doi:10.1158/1055-9965.EPI-20-0269
35. Patel K, Beheshti A. Call to action. Presented at: Long COVID and Cancer Conclave Meeting; May 12, 2023; Accessed via email June 19, 2023. Charlotte, NC.
Articles in this issue
over 2 years ago
FROM THE EDITOR IN CHIEF: Days of Future Pastover 2 years ago
Perspectives on EOM: What Makes Sense Moving Forwardover 2 years ago
Business Highlights From Partners in Community Oncologyover 2 years ago
Coverage in Health Equity: October 2023over 2 years ago
Why Failing Faster Is the Key to Accelerating Drug DiscoveryNewsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.