Video
Overview of Basal Cell Carcinoma
An overview of basal cell carcinoma considering differential diagnoses and the current standard of care.
Transcript
Morgana Freeman, MD: Basal cell carcinoma is the most common cancer diagnosed in the United States. There were about 4 million cases diagnosed last year, and the incidence has gone up a little over 200% in the last 3 decades. It’s primarily a UV [ultraviolet light]-induced cancer, typically a cancer that occurs in older patients. Most of the time this presents on sun-exposed areas, primarily on the head and neck. In some cases, there can be an inherited tendency to develop basal cell carcinoma such as Gorlin syndrome, but the majority of the cases that we see are those that are UV-induced. Most of the time, they are highly curable. There’s a very low metastatic rate, less than 1%, according to the most recent SEER [Surveillance, Epidemiology, and End Results] data. These are typically again managed by Mohs surgery or other topical agents.
The majority of basal cell carcinoma will present as a single, small pearly pink lesion or papule, again typically near the nose, somewhere on the face, sometimes on the scalp, and in some cases, below the head and neck—on the shoulders or the back. In cases where the patient neglects the lesion, it can become very large or very fungating and erode deep tissues. Unfortunately, I’ve seen patients in my clinical practice who have done this where it’s a tumor of neglect, and the simple excision or Mohs surgery is simply not possible. The great majority of cases are limited and very small in size.
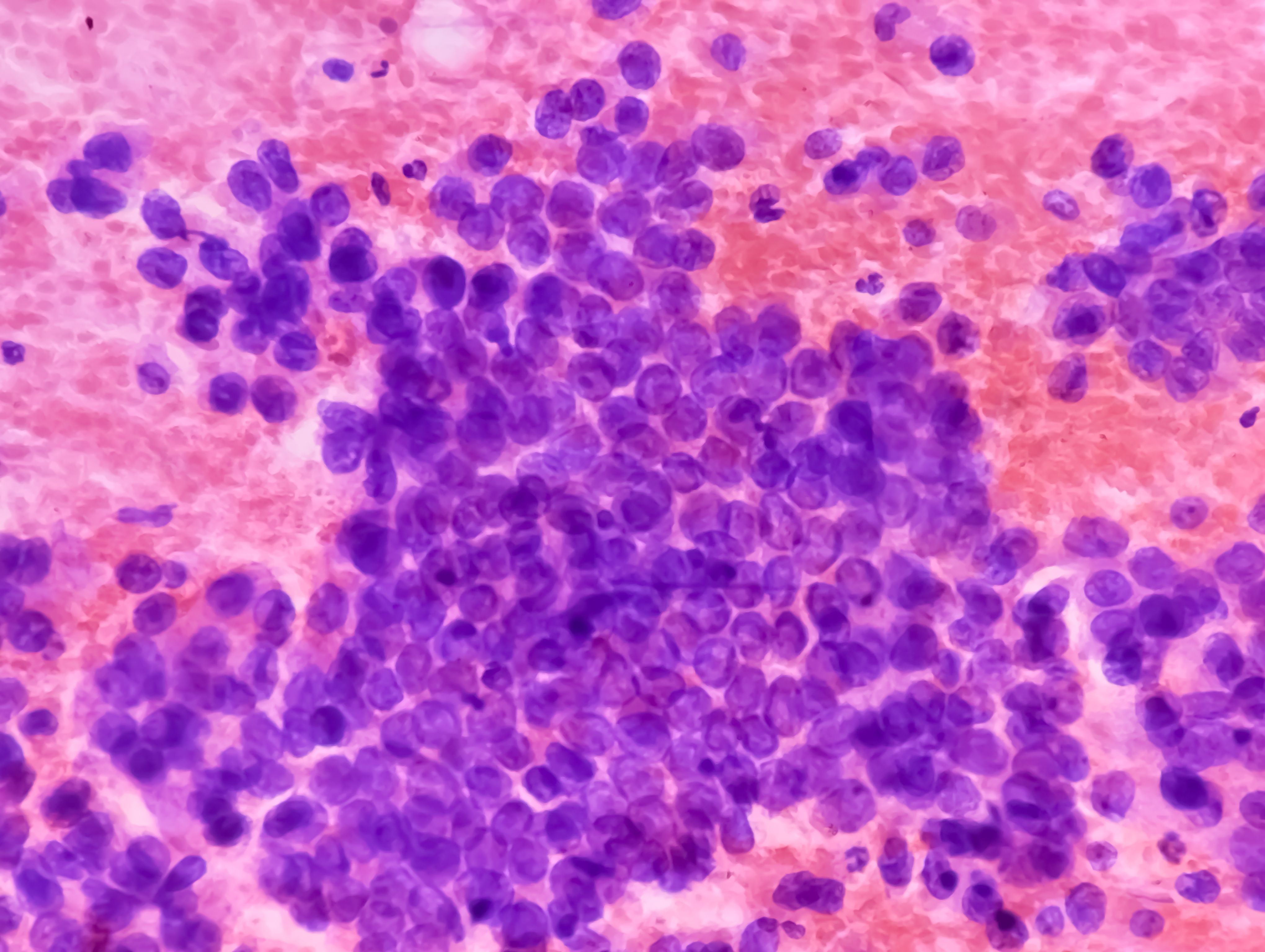
When a patient presents with a pearly pink lesion, and in some cases it may be painless, somewhere on the face, obviously biopsy is the right way to go. The majority of these cases are detected by the patient’s dermatologist or primary care physician. Other differential diagnoses to consider are, of course, amelanotic melanoma, squamous cell carcinoma, or Merkel cell carcinoma. Any time the patient presents with a rounded papule lesion, obviously biopsy is needed. This is not something you simply manage by visible diagnosis alone. You need biopsy for confirmation.
Omid Hamid, MD: The NCCN [National Comprehensive Cancer Network] guidelines for basal cell carcinoma recommend resection and excision of the basal cell carcinoma. That is, the majority of basal cell carcinomas are easily manageable by a local resection and have high rates of cure. That would be either through a surgical excision or evaluation by a dermatologist who’s experienced in Mohs micrographic surgery.
My first line of therapy for basal cell carcinoma is to evaluate if it’s surgically resectable, and then have a discussion with a surgical oncologist or a Mohs micrographic surgeon. In areas where surgery may be contraindicated, those are specific areas that would cause deformity or loss of function. It would be near the eyelid or other areas. We would talk about local radiation. We would also possibly talk about some of the topical agents with a close follow-up.
Morgana Freeman, MD: Following simple excision, there are other treatment modalities that can be employed. In many cases, Mohs is again the most often opted for surgical option. Photodynamic therapy is not something typically used. We use that more from a preventive standpoint or thinking about management of AKs [actinic keratoses]. Some dermatologists will elect to use topical imiquimod, especially if there’s some concern potentially that there are deeper layers of skin that are involved or couldn’t fully be excised by Mohs. Of course, in cases where it’s a very large tumor or there are some risk factors for recurrence, if it has a desmoplastic or infiltrative pattern, if there’s evidence of perineural invasion, or lymphatic invasion, that patient may be referred for adjuvant radiation therapy. There are also, of course, cases of large tumors that may be neglected, and we use neoadjuvant radiation therapy to help shrink that tumor and make them a more appropriate surgical candidate.
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.