- February 2023
- Volume 29
- Issue 2
- Pages: SP134-SP138
Recent FDA Actions: February 2023
FDA Approves Zanubrutinib for First-line R/R CLL/SLL
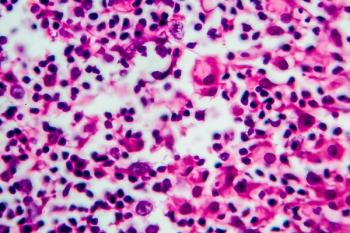
The FDA approved the Bruton tyrosine kinase (BTK) inhibitor zanubrutinib (Brukinsa; BeiGene) on January 19 for all patients with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL), whether newly diagnosed or previously treated for the disease—including those who have received ibrutinib (Imbruvica).1
Ibrutinib, a first-generation BTK inhibitor, created a sea change in treating CLL when it was approved in 2014. Broad approval for zanubrutinib in CLL promises a new milestone in treating patients with the disease, which accounts for one-fourth of all US leukemia cases.2 In an email to The American Journal of Managed Care®, Jennifer R. Brown, MD, PhD, the lead investigator for the study showing zanubrutinib’s superiority over ibrutinib, said she expected a rapid shift to zanubrutinib, with no resistance from payers.
The approval could affect up to estimated 21,000 patients in the United States who will receive a diagnosis of CLL or SLL in 2023, according to the American Cancer Society.2 It follows the December 13, 2022, presentation of data from the phase 3 ALPINE trial (NCT03734016) at the 64th American Society of Hematology (ASH) Annual Meeting.3 The data also were published in the New England Journal of Medicine.4 Study results showed that after 2.5 years zanubrutinib offered a 35% benefit in progression-free survival (PFS) over ibrutinib among patients with relapsed/refractory (R/R) disease, and the edge widened among higher-risk patients (HR, 0.65; 95% CI, 0.49-0.86; P = .002).
In ALPINE, efficacy among 652 patients was evaluated based on overall response rate (ORR) and duration of response (DOR), as determined by an independent review committee. The ORR was 80% (95% CI, 76%-85%) in the zanubrutinib arm and 73% (95% CI, 68%-78%) in the ibrutinib arm for a response rate ratio of 1.10 (95% CI, 1.01-1.20; P = .0264). The median DOR was not reached in either arm after a median follow-up of 14.1 months.
The FDA approval also covers patients previously untreated for CLL/SLL, based on results from the phase 3 SEQUOIA trial (NCT03336333), which were presented at the 2022 European Hematology Association Congress. In that study, the median PFS was not reached in the zanubrutinib arm. However, patients receiving a combination bendamustine plus rituximab had a PFS of 33.7 months (HR, 0.42; 95% CI, 0.28-0.63, P < .0001).1
In SEQUOIA, a nonrandomized cohort of previously untreated patients with CLL/SLL and 17p deletion were also evaluated. The ORR was 88% (95% CI, 81%-94%), and the median DOR was not reached after a median follow-up of 25.1 months.
Zanubrutinib was previously approved in the United States to treat smaller patient groups with mantle cell lymphoma, marginal zone lymphoma, and those with Waldenström macroglobulinemia.
Brown, director of the CLL Center at Dana-Farber Cancer Institute in Boston, Massachusetts, who presented the ALPINE data at ASH, had predicted that the FDA’s label would be broad.
In an emailed statement, Brown said ALPINE “found that zanubrutinib led to fewer [adverse] effects and adverse events than ibrutinib, leading to a better quality of life for patients. I am encouraged that zanubrutinib has been approved for adult patients with CLL and SLL and optimistic that many patients across the country will benefit from this approval.”
Zanubrutinib’s benefit over ibrutinib is seen as 2-fold. It offers superior responses and fewer adverse effects, because this second-generation therapy has “greater BTK specificity than ibrutinib,” Brown explained during her ASH presentation. Its higher concentration allows for more sustained BTK inhibition, and its improved mechanism reduces off-target cardiac effects, allowing patients to stay on therapy longer.
In fall 2022, the National Comprehensive Cancer Network (NCCN) listed zanubrutinib as a preferred agent over ibrutinib in CLL in its guidelines, based on zanubrutinib’s improved safety profile.5
During ASH, Brown told reporters she could not think of a patient group that should be prescribed ibrutinib instead of zanubrutinib. She repeated that recommendation in a follow-up email when asked if she expected rapid adoption of zanubrutinib.“I certainly hope that clinicians will move quickly to Brukinsa, given that it demonstrated improved efficacy and safety compared to Imbruvica,” Brown said. “There is no situation in which I would start a patient on ibrutinib anymore.”
Asked if she anticipated any payer resistance to coverage in in CLL, Brown said, “No, not with the approval and the NCCN listing. Payers are already quite adapted to BTK inhibitors in first-line CLL.”
References
1. FDA approves zanubrutinib for chronic lymphocytic leukemia or small lymphocytic leukemia. News release. FDA. January 19, 2023. Accessed January 19, 2023. http://bit.ly/3WrqH0A
2. Key statistics for chronic lymphocytic leukemia. American Cancer Society. January 12, 2023. Accessed January 19, 2023. http://bit.ly/3uZtUJv
3. Brown JR, Eichhorst B, Hillmen P, et al. Zanubrutinib demonstrates superior progression-free survival (PFS) compared with ibrutinib treatment of relapsed/refractory chronic lymphocytic leukemia and small lymphocytic lymphoma (R/R CLL/SLL): results from final analysis of ALPINE randomized phase 3 study. Presented at: 64th American Society of Hematology Annual Meeting & Exposition; New Orleans, LA; December 10-13, 2022; Abstract LBA-6.
4. Brown JR, Eichhorst B, Hillmen P, et al. Zanubrutinib or ibrutinib in relapsed or refractory chronic lymphocytic leukemia. N Engl J Med. Published online December 13, 2022. doi:10.1056/NEJMoa2211582
5. Caffrey M. NCCN update moves zanubrutinib ahead of ibrutinib in CLL/SLL based on toxicity profile. Am J Manag Care. 2022;28(Spec 7):SP427.
FDA Approves Bispecific Antibody Mosunetuzumab for R/R Follicular Lymphoma
The FDA has approved mosunetuzumab-axgb (Lunsumio; Genentech), a bispecific antibody for the treatment of adults with relapsed/refractory follicular lymphoma (R/R FL) after 2 or more prior lines of systemic therapy.
Mosunetuzumab had been granted priority review for R/R FL in July 2022.
The December 23, 2022, decision was supported by data from the phase 2 GO29781 study (NCT02500407), which demonstrated high and durable response rates. As this is an accelerated approval, continued approval may be contingent on the verification of clinical benefit in a confirmatory trial.1
Mosunetuzumab is the first of its class approved to treat FL. Bispecific antibodies aim at 2 targets, increasing their potency against cancer. These are off-the-shelf products, as opposed to chimeric antigen receptor (CAR) T-cell therapies, which are personalized.
“This approval is a significant milestone for people with relapsed or refractory follicular lymphoma, who have had limited treatment options until now,” Elizabeth Budde, MD, PhD, a Lunsumio clinical trial investigator, said in a statement.1 “As a first-in-class, T-cell engaging, bispecific antibody that can be initiated in an outpatient setting, Lunsumio’s high response rates and fixed duration could change the way advanced follicular lymphoma is [managed].” Budde is a hematologic oncologist and associate professor in the Division of Lymphoma, Department of Hematology & Hematopoietic Cell Transplantation, at City of Hope in Duarte, California.
After a median of 28.3 months of follow-up, 60% of patients with 2 or more prior therapies experienced a complete response (CR) (95% CI, 49.1%-70.2%) and 77.8% achieved an objective response, which includes CR plus partial responses (95% CI, 67.8%-85.9%), according to data presented at the 2022 American Society of Hematology Annual Meeting & Exposition, held in December in New Orleans, Louisiana.2
Furthermore, 62.7% of patients who achieved CR were still in remission after 24 months (95% CI, 37.7%-87.7%). Nearly half (48.3%) of patients remained progression free (95% CI, 36.2%-60.5%).
The most common adverse event (AE) was cytokine release syndrome (CRS), which occurred in 38% of patients for a median duration of 3 days. CRS can be severe and life-threatening and is also a common AE of CAR T-cell therapies. Other common AEs that occurred in 20% or more patients were fatigue, rash, pyrexia, and headache.
Prior to the approval, Nancy L. Bartlett, MD, Koman Chair in Medical Oncology at Washington University School of Medicine in St Louis, Missouri, wrote in an editorial in New England Journal of Medicine that “bispecific agents will be an excellent option for the 60% of patients in whom second-line CAR T-cell therapy fails.”3 Bartlett presented the phase 2 data on mosunetuzumab at the annual meeting.
Mosunetuzumab is delivered as an intravenous infusion for a fixed duration and can be infused in the outpatient setting. Hospitalization for select AEs may be necessary, and hospitalization is recommended for infusions after a grade 3 CRS event and should be considered after a grade 2 CRS event.
“This additional treatment option is good news for people whose blood cancer has not responded to multiple lines of treatment because it can become more difficult to treat each time it returns,” Lee Greenberger, PhD, chief scientific officer of the Leukemia & Lymphoma Society, said in the statement.1 “This bispecific antibody is an off-the-shelf, accessible treatment option that has the potential to help those with relapsed or refractory follicular lymphoma achieve remission.”
References
1. FDA approves Genentech’s Lunsumio, a first-in-class antibody, to treat people with relapsed or refractory follicular lymphoma. News release. Genentech. December 23, 2022. Accessed January 4, 2023. https://bit.ly/3BT9Exa
2. Bartlett NL, Sehn LH, Matasar MJ, et al. Mosunetuzumab monotherapy demonstrates durable efficacy with a manageable safety profile in patients with relapsed/refractory follicular lymphoma who received ≥2 prior therapies: updated results from a pivotal phase II study. Presented at: 64th American Society of Hematology Annual Meeting & Exposition; December 9-13, 2022; New Orleans, Louisiana. Abstract 610. https://ash.confex.com/ash/2022/webprogram/Paper157691.html
3. Bartlett NL. Bispecific antibodies in lymphoma - another win for T cells. N Engl J Med. 2022;387(24):2285-2286. doi:10.1056/NEJMe2212732
Tucatinib Plus Trastuzumab Is Approved for RAS Wild-type, HER2+ Unresectable or Metastatic Colorectal Cancer
The combination of tucatinib (Tukysa) and trastuzumab has received accelerated approval from the FDA to treat adults with RAS wild-type, HER2-positive unresectable or metastatic colorectal cancer (mCRC) that advances after treatment with specific types of chemotherapy.
FDA’s January 19, 2023, approval of this chemotherapy-free combination is based on results from the phase 2 MOUNTAINEER trial (NCT03043313), which found a 38% overall response rate (95% CI, 28%-49%) among 84 patients, based on a blinded independent central review. Complete responses were seen in 3.6% (n = 3 patients) and partial responses were seen in 35% (n = 29). The median duration of response was 12.4 months (95% CI, 8.5-20.5).1
Data for MOUNTAINEER were presented in July 2022 at the European Society for Medical Oncology World Congress on Gastrointestinal Cancers.
CRC is among the more common cancers in the United States, with the American Cancer Society estimating about 153,000 individuals will receive a diagnosis in 2023.2 Rates are increasing among younger adults, with experts attributing this to rising rates of obesity. Approximately 22% of those with a diagnosis already have advanced cancer; HER2 is overexpressed in 3% to 5% of patients, and 10% have RAS wild-type mCRC.3
Tucatinib, available in tablets of 50 or 150 mg, is an oral tyrosine kinase inhibitor of the HER2 protein. It blocks phosphorylation of HER2 and HER3, which results in inhibition of downstream mitogen-activated protein kinase and AKT signaling and cell growth, as well as antitumor activity. It was approved in April 2020 in combination with trastuzumab and capecitabine to treat adults with advanced unresectable or metastatic HER2-positive breast cancer if they have received at least 1 prior anti-HER2–based regimen for metastatic disease.
“Historically, patients with HER2-positive metastatic colorectal cancer who have progressed following frontline therapy have had poor outcomes,” John Strickler, MD, associate professor of medicine, Duke University Medical School in Durham, North Carolina, and lead investigator for the MOUNTAINEER trial, said in a statement.4 “The FDA approval of a chemotherapy-free combination regimen that specifically targets HER2 is great news for these patients.”
Biomarker testing now allows clinicians to identify patients with RAS wild-type HER2-positive disease. Michael Sapienza, CEO of the Colorectal Cancer Alliance, emphasized the need for both doctors and patients to embrace comprehensive biomarker testing at diagnosis, “because it can inform treatment decisions and help improve outcomes.”
Adverse events (AEs) reported during the MOUNTAINEER trial—and included in prescribing warnings—included diarrhea, hepatoxicity, and embryo-fetal toxicity (although no human data are available regarding fetal harm). In MOUNTAINEER, serious AEs occurred in 22% of patients, with the most common being intestinal obstruction (7%), urinary tract infection (3.5%), pneumonia, abdominal pain, and rectal perforation (2.3% each).
Common AEs from the regimen were diarrhea, fatigue, rash, nausea, abdominal pain, infusion-related reactions, and pyrexia, each affecting at least 20% of participants. AEs led to discontinuation of tucatinib in 6% of participants.
References
1. Strickler JH, Cercek A, Siena S, et al: MOUNTAINEER: open-label, phase 2 study of tucatinib in combination with trastuzumab for HER2-positive metastatic colorectal cancer. ESMO World Congress on Gastrointestinal Cancers 2022. Abstract LBA-2. Presented July 2, 2022. http://bit.ly/3WsuQl0
2. Key statistics for colorectal cancer. American Cancer Society. January 13, 2023. Accessed January 19, 2023. https://www.cancer.org/cancer/colon-rectal-cancer/about/key-statistics.html
3. Wang J, Li S, Liu Y, Zhang C, Li H, Lai B. Metastatic patterns and survival outcomes in patients with stage IV colon cancer: A population‐based analysis. Cancer Med. 2020;9(1):361-373. doi:10.1002/cam4.2673
4. Seagen announces FDA accelerated approval of Tukysa (tucatinib) in combination with trastuzumab for people with previously treated RAS wild-type, HER2-positive metastatic colorectal cancer. News release. Seagen. January 19, 2023. http://bit.ly/3XFJjv1
Articles in this issue
almost 3 years ago
Our Rashomon Momentalmost 3 years ago
Managed Care & Clinical Updates: February 2023almost 3 years ago
From Our Partners: February 2023almost 3 years ago
Finding Quality in Cancer Care Beyond the Hospital Wallsalmost 3 years ago
Center on Health Equity & Access: February 2023Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.