
Research has uncovered 2 pathways through which lung adenocarcinoma can develop, and that knowledge could help target treatments to patients who will benefit the most, according to a new study published in Cancer Cell.

Laura Joszt, MA, is the vice president of content for the managed care and pharmacy brands at MJH Life Sciences®, which includes The American Journal of Managed Care®, Managed Healthcare Executive®, Pharmacy Times®, and Drug Topics®. She has been with MJH Life Sciences since 2011.
Laura has an MA in business and economic reporting from New York University. You can connect with Laura on LinkedIn or Twitter.

Research has uncovered 2 pathways through which lung adenocarcinoma can develop, and that knowledge could help target treatments to patients who will benefit the most, according to a new study published in Cancer Cell.

The brain shrinkage that occurs in patients with multiple sclerosis may be the result of a specific brain cell: When projection neurons are damaged, the brain shrinks.

A case study from The Ohio State University highlights how initiatives addressed system-level drivers of burnout and not only improved the health of faculty, staff, and students, but also saved money.

Some cancers, such as breast cancer and leukemia, were well-funded compared with their incidence, mortality, and person-years of life lost, while others, such as gastrointestinal and brain cancers, were all poorly funded.

While poor sleep quality is common in patients with interstitial lung disease (ILD), it is unclear which factors other than sleep disordered breathing may contribute to poor sleep quality for these patients. A study published in ERJ Open Research found that providers should target depression and coexisting sleep disorders in order to improve sleep quality and quality of life for patients with ILD.

When it comes to performing high-risk procedures, the majority of hospitals do not perform them often enough to meet safety standards, according to a new report from The Leapfrog Group.
Venous thromboembolism (VTE) is a significant complication for patients with multiple myeloma (MM) who are being treated with immunomodulatory drugs (IMiDs), and a new assessment model may help to predict VTE in this population.

Panelists at the National Alliance of Healthcare Purchaser Coalitions' Leadership Summits highlighted the ways their companies are customizing care and benefits to meet the needs of their employees.

An anaysis of nontuberculous mycobacterial (NTM) diagnostic tests for 15 years, water disinfection treatment, and water sources has found that where a city gets it water can increase the risk of NTM infection more than how the water is treated.

Financial toxicity, ACO contracts, removing barriers to care.

Patients with obesity not only have a higher risk of pediatric multiple sclerosis (MS), but they also do not respond as well to first-line medications.

Two reports from the Office of Inspector General (OIG) in HHS have identified deficiencies in the quality of care at hospices and the harm done to beneficiaries as a result of poor care or cases of abuse.

A poster abstract evaluated real-world treatment patterns by region and age to better understand these issues in order to address them.

HHS Secretary Alex Azar's proposed rule to eliminate drug rebates and pass discounts directly to the patient is getting dropped by the White House.

As social determinants of health are being more intensely researched, one determinant that is already well understood and has a number of interventions in place and being studied is housing. Here are 5 things about housing in healthcare.

Some generic drugs may actually cost Medicare Part D beneficiaries more out-of-pocket than brand-name drugs because brand-name manufacturers can offer discounts that generic drug makers cannot pay.
Achieving undetectable minimal residual disease (MRD) status is important for deep and durable responses in patients with chronic lymphocytic leukemia (CLL), according to 2 abstracts presented at the 2019 American Society of Clinical Oncology Annual Meeting.
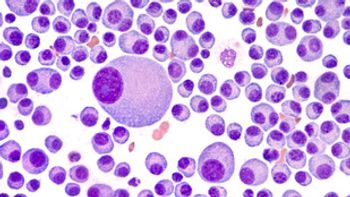
While minimal residual disease (MRD) is being used to assess response to treatment in multiple myeloma (MM), the level of risk a patient has can make a big different in how well MRD works as a prognostic indicator, according to 2 abstracts presented at the 2019 American Society of Clinical Oncology Annual Meeting.

Although health equity has been a stated public health goal, new research shows that there has been a lack of progress on health equity in the last 25 years in the United States, indicating that the country must either work harder to promote health equity or must find out which policies would produce greater improvements in health equity.

Bringing together different stakeholders in healthcare to share the challenges they see and their own understanding of how to fix the problem can help make impossible things happen and bring change to the healthcare system, said Elizabeth Mitchell, president and chief executive officer, Pacific Business Group on Health.

Treating illnesses is important, but it would be a mistake to think that is the full extent of health. Panelists during the National Alliance of Healthcare Purchaser Coalitions’ 2019 Leadership Summits, held June 24-26 in Pittsburgh, Pennsylvania, discussed the impact of social determinants and past trauma on health and how employers can ensure they are addressing these issues to improve health and outcomes.

Postural sway, the tendency to sway even while standing still, is an independent risk factor for bone fractures in postmenopausal women.



Patients with pediatric-onset multiple sclerosis (MS) not only have lower cognitive scores in adulthood than patients with adult-onset MS, but cognitive scores declined faster.

Coverage from The American Journal of Managed Care's® Institue for Value-Based Medicine® meetings.

Bone is one of the most frequent sites of metastasis in breast cancer, but the exact reasons for this high risk of bone metastases has not been well understood. However, research has found that physics may be partly the reason for this high risk.

Currently, the number of patients who are actually utilizing precision cancer care treatments is small, but it is growing fast. As that happens, physicians will need to get comfortable with ordering the right tests, explained Clynt Taylor, chief executive officer of Intervention Insights, and Lee Newcomer, MD, formerly of UnitedHealth Group.

The FDA is partnering with COTA, a precision medicine technology company, to gain better insight into treatment variation within subpopulations of patients using real-world data. The program will start with breast cancer and may expand to other cancer types.

259 Prospect Plains Rd, Bldg H
Cranbury, NJ 08512
© 2025 MJH Life Sciences®
All rights reserved.
