
An investigation into the effects of a self-management intervention (SMI) called “Better Living with COPD” found that the intervention had a significant positive short-term effect for patients with chronic obstructive pulmonary disease.


An investigation into the effects of a self-management intervention (SMI) called “Better Living with COPD” found that the intervention had a significant positive short-term effect for patients with chronic obstructive pulmonary disease.

It is already well established that patients with COPD have exacerbations during winter as well as during heat waves in the summer months, and researchers in Germany sought to see which patient groups might be potentially more vulnerable to the effects of climate change in order to see who might need targeted care.

Retraction and republication: The JAMA article referenced in this story was retracted and republished on October 8, 2019. Please refer to the updated findings here.

The FDA approved revefenacin (Yupelri), the first once-a-day nebulized bronchodilator for the treatment of chronic obstructive pulmonary disease (COPD).

Inhaled corticosteroids, used for preventing acute exacerbation of chronic obstructive pulmonary disease (COPD), often lead to increased high blood eosinophil count, while low blood eosinophil count is often associated with pneumonia risk—however, the prognostic role of blood eosinophil count has not yet been explored. In a recent study, researchers found that the severity of emphysema was independently linked with low blood eosinophil count and the longer survival period was associated with increased blood eosinophil count.

Researchers recently studied the adverse outcomes of symptomatic and asymptomatic nonobstructed individuals and those with mild chronic obstructive pulmonary disease (COPD) longitudinally, and found that the presence of respiratory symptoms in nonobstructed individuals was a predictor of mortality, lung function decline, and exacerbations.
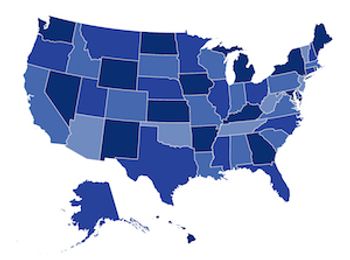
A new report on the prevalence of chronic obstructive pulmonary disease (COPD) shows that there is wide variability across and within states, with West Virginia carrying the highest burden of morbidity and mortality.

Researchers reviewed the most updated concepts of the pulmonary vascular changes in chronic obstructive pulmonary disease (COPD) and concluded that certain subgroups of COPD patients with pulmonary vascular phenotypes may profit from targeted pulmonary arterial hypertension therapy.

Researchers looked to evaluate predictors of mortality in patients with COPD after 9 years.

The first trial to examine the impact of a self-management behavior-modification program combined with bronchodilator therapy and exercise training on exercise capacity and physical activity in patients with chronic obstructive pulmonary disease (COPD) showed positive results, according to a recently published study.

Oral theophylline has been used as a bronchodilator to treat chronic obstructive pulmonary disease (COPD) for decades, but it has fallen out of favor due to the side effects that come with the higher doses that are required to achieve any beneficial effect. A recent study sought to determine if adding low-dose theophylline to inhaled corticosteroids for COPD would reduce the number of exacerbations.

A recent study determined that patients with chronic obstructive pulmonary disease (COPD) and non-small cell lung cancer (NSCLC) had similar tumor microenvironment, but higher tumor infiltrating lymphocytes (TIL) exhaustion, than patients without COPD. The use of an anti-programmed cell death-1 (PD-1) antibody, nivolumab, was also demonstrated to be effective in this population.

Some patients with chronic obstructive pulmonary disease (COPD) experience a sudden worsening of their symptoms that require additional treatment—also known as acute exacerbation of COPD (AECOPD). A recent study, which investigated whether readmissions of patients with severe AECOPD varied according to the bacterium or virus identified, found that P. aeruginosa identification is associated with a higher readmission rate in patients.

Previous phase 3 studies have demonstrated the efficacy of nebulized glycopyrrolate inhalation solution (GLY) for treating patients with chronic obstructive pulmonary disease (COPD). In a recent study, researchers conducted a secondary analysis and found that nebulized GLY demonstrated efficacy and was well tolerated for up to 48 weeks in subjects with COPD with or without background long-acting beta2-agonist (LABA).

Patient adherence to medication is a complex issue, particularly so for patients with chronic obstructive pulmonary disease (COPD). A recent study finds that adherence is related to need perception and to the functional severity of the disease.

Patients with chronic obstructive pulmonary disease (COPD) often have a significant disease burden that is particularly associated with the peak incidence of exacerbation events during winter months. A review assessed previous population studies that evaluated the impact of seasonality in COPD, emphasizing the importance of understanding how all factors impact patients and where interventions can be targeted.

Older age, dyspnea, longer duration of illness, comorbidities, and use of oxygen hurt quality of life for those with chronic obstructive pulmonary disease.
A Mayo Clinic team critiqued the 2018 update to the Global Initiative for Chronic Obstructive Lung Disease guidelines, recommending several changes to the next update.

A study found that testosterone replacement therapy reduced the risk of respiratory hospitalizations in men with chronic obstructive pulmonary disease (COPD).

A phase 2 clinical trial of a surgical procedure called targeted lung denervation to open blocked airways in patients with chronic obstructive pulmonary disease (COPD) showed that it reduced problems associated with the disease.

There is an increased need for potential biomarkers that can identify patients with chronic obstructive pulmonary disease (COPD) who will benefit from treatment involving inhaled corticosteroids (ICS). According to a recent study, the 2% threshold for blood eosinophils could accurately predict ICS treatment response in patients with COPD, but the risk of pneumonia was increased.

Autoimmunity plays a role in the development of chronic obstructive pulmonary disease (COPD), according to a recent genome study.

Telerehabilitation (TR), defined as telecare that involves supervised online exercise sessions for patients with chronic obstructive pulmonary disease (COPD), is beneficial for symptom relief, physical function, and quality of life. A recent study found that specific attention toward the involvement of health professionals in the decision process combined with education and skill training is essential to support the successful implementation of TR.

Early hospital readmissions for patients with asthma and chronic obstructive pulmonary disease (COPD) represent a major economic burden within the healthcare system and recent research found that comorbid chronic rhinitis is significantly associated with 30-day asthma and COPD related readmissions

Patients with chronic obstructive pulmonary disease (COPD) still rely on their healthcare providers as the source of primary information about their disease but about a third will bring information from the internet to appointments to discuss, and prioritize information about symptom control, a recent online survey reported.

259 Prospect Plains Rd, Bldg H
Cranbury, NJ 08512
© 2025 MJH Life Sciences®
All rights reserved.
