
With President Joe Biden marking his 100th day in office at the end of the month, a health policy strategist sat down for a conversation to discuss the new administration’s achievements and challenges.

Half of US adults have been administered 1 COVID-19 vaccine dose; researchers identify cause of clotting events associated with AstraZeneca vaccine; Anthony Fauci, MD, the chief medical advisor to the president, says he believes a decision on whether to resume the J&J vaccine will come by Friday.

With President Joe Biden marking his 100th day in office at the end of the month, a health policy strategist sat down for a conversation to discuss the new administration’s achievements and challenges.

Study quantifies risk of blood clots in patients with COVID-19; Biden administration aims to reverse restrictions on fetal tissue research; Michigan hospitals struggle to care for COVID-19 cases.

A poster at the Academy of Managed Care Pharmacy 2021 meeting examined the impact of high-deductible health plans (HDHPs) on access to health care and resource use in the United States and the interaction of race, ethnicity, and income.

The pandemic reduced visits to specialists last year, which in turn reduced the volume of prescriptions, according to a presentation at the Academy of Managed Care Pharmacy 2021 meeting.

New research presented at AMCP 2021, the annual meeting of the Academy of Managed Care Pharmacy, evaluated treatment patterns and costs related to hospitalization for patients with pulmonary arterial hypertension (PAH).

The CDC's Advisory Committee on Immunization Practices (ACIP) declined to change the current recommendation to pause administration of Johnson & Johnson's COVID-19 vaccine.

Compared with when Medicare Part D launched, therapies today are more expensive. A panel at the Academy of Managed Care Pharmacy 2021 meeting discussed how the benefit needs to adapt to keep up with the future.

For some living with HIV, old wounds have reopened during the COVID-19 pandemic, explained Perry N. Halkitis, PhD, MS, MPH, dean of the Rutgers School of Public Health and director of the Center for Health, Identity, Behavior and Prevention Studies.

After cases of rare and severe blood clots led to 1 death and 1 hospitalization, the CDC and FDA will pause the use of Johnson & Johnson's (J&J) COVID-19 vaccine.

Adverse reactions to the Johnson & Johnson vaccine cause some states to pause distribution; the Biden administration proposes creation of a $6.5 billion medical research agency aiming to cure cancer and other diseases; Pfizer/BioNTech seeks expansion of its COVID-19 vaccine emergency use authorization in adolescents.

Every week, The American Journal of Managed Care® recaps the top managed care news of the week, and you can now listen to it on our podcast, Managed Care Cast.
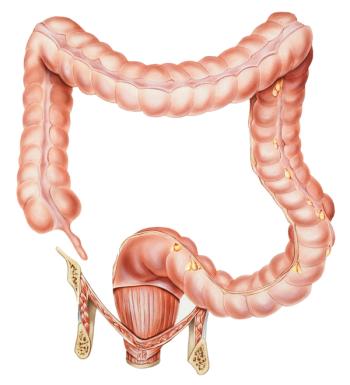
The device, which highlights for gastroenterologists regions of the colon that have visual characteristics consistent with possible cancerous abnormalities, is already in use in Europe.

A high proportion of Marshallese, or Marshall Islanders, living on the mainland Unites States, have undiagnosed hypertension and type 2 diabetes (T2D), according to findings that will be used to address disparities in Native Hawaiian and Pacific Islander populations.

The findings illustrate the importance of prioritizing COVID-19 vaccinations for patients on dialysis.

On day 2 of this year’s Community Oncology Conference, a panel of government and health policy experts gathered to discuss the hot-button issue of political influence on cancer policy and the damage community oncology has suffered this past year.

There are many sources, and definitions, of where the value in cancer care lies. In this panel discussion, a cancer survivor and patient advocate, an oncologist, and a benefits professional provided their perspectives on what value in cancer care means to them.

A 2021 survey on health care trends to monitor finds provider burnout, disengagement, and shortage of health care professionals as the most potentially disruptive issues facing hospitals and health systems in the next 3 years.

Lalan Wilfong, MD, executive vice president, Value Based Care & Quality Programs, Texas Oncology, and cochair, Payment Reform, Community Oncology Alliance, speaks on the evolution of remote monitoring in cancer care and how value-based oncology may look in the near future.
Edward Licitra, MD, PhD, medical oncologist, Astera Health Partners, discusses his thoughts on what value-based cancer care entails and how physicians can best align their goals with those of the patient and health plan.

Coverage of our peer-reviewed research and news reporting in the health care and mainstream press.

A popular misconception of palliative care is that it only has importance toward making patients comfortable at the end of their lives, noted a palliative care physician on the first day of the 2021 Community Oncology Conference, presented by the Community Oncology Alliance.

Ted Okon, MBA, executive director of the Community Oncology Alliance, discusses what influence the new administration may have on payment reform in oncology and issues regarding the 340B drug pricing program.

Officials urge the Biden administration to track COVID-19 deaths among health care workers; the B.1.1.7 variant is now the dominant strain in the United States; pandemic results in steep declines in STD testing.

Prioritization, interunit collaboration, esprit de corps, and health workers’ adaptability are key factors in providing a coherent response to the coronavirus disease 2019 pandemic.

Jeff Patton, MD, CEO, OneOncology, and chairman of the board, Tennessee Oncology, discusses what influence COVID-19 will have on discussions at the Community Oncology Conference 2021, as well as takeaways he hopes audience members and participants gain from the conference.

259 Prospect Plains Rd, Bldg H
Cranbury, NJ 08512
© 2025 MJH Life Sciences®
All rights reserved.
