Payers
Latest News

Latest Videos

CME Content
More News

Physicians and health care groups have lined up to support the Value in Health Care Act, which could create new incentives to adopt value-based care.

The playbook from the 3 organizations highlights 5 best practices for data sharing from organizations with real-world experience in value-based care arrangements.

Despite having 8 adalimumab biosimilars on the market now, patients may only see 1 or 2 available through their insurance, explained Laura Wingate, executive vice president, Education, Support, & Advocacy, Crohn's & Colitis Foundation.

A new analysis finds branded insulin glargine (Lantus) still has a majority of total market volume and new drug starts despite competition from Semglee, an interchangeable biosimilar.

An online survey identified that documentation requirements and communication issues with health plans are associated with providers modifying clinical decisions to avoid medication prior authorization.

Medication formulary policies represent a key determinant of access to medication and can be leveraged to advance pharmacoequity and health equity writ large.

After the Supreme Court ruled reimbursement cuts to 340B hospitals were done unlawfully, CMS is proposing to repay hospitals and providers in the program with a lump sum that has repercussions for other hospitals because of the agency’s need to be budget neutral.

Two abstracts presented at the 2023 American Society of Clinical Oncology annual meeting evaluated biosimilar adoption across oncology practices and highlighted the role payers play in preventing or promoting adoption.

After 7 years, competition for Humira is here. The first adalimumab biosimilar launched in January, but an additional 8, including an interchangeable product, will hit the US market in July.

The Act4Biosimilars Action Plan seeks to increase biosimilar adoption by at least 30 percentage points in 30-plus countries by 2030.

Officials note it could slow acquisition of physicians’ offices, but hospitals bristle at prospect.
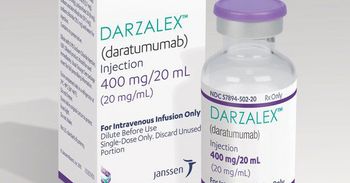
A second study will evaluate the treatment and financial burden and quality of life of a program of subcutaneous daratumumab administered at home.
Michael Thompson, president and CEO of the National Alliance of Healthcare Purchaser Coalitions, gave insight into the themes of the upcoming National Alliance Leadership Summits.

The pharmacy benefit manager SmithRx has announced that through a partnership with the Mark Cuban Cost Plus Drug Company, it will offer Yusimry, an adalimumab biosimilar, for less than 90% of the cost of the reference product, Humira.

According to a spokesperson, Merck is prepared to take the lawsuit to the Supreme Court as it challenges drug price negotiations as part of the Inflation Reduction Act.

The FDA approved Pfizer’s respiratory syncytial virus (RSV) vaccine Wednesday; Medicare announced plans to largely cover a new class of expensive Alzheimer drugs; more states are extending postpartum coverage under Medicaid.

Insurance is by far the most important factor of whether patients followed up with treatment after getting screened for glaucoma, said Byron L. Lam, MD, professor of ophthalmology, University of Miami Miller School of Medicine's Bascom Palmer Eye Institute.

Kicking off the 2023 Greater Philadelphia Business Coalition on Health annual conference, Mark Fendrick, MD, of the University of Michigan, delivered a keynote exhorting the audience of employers and payers to implement the principles of value-based insurance design (VBID) in order to improve individual and population health and drive toward equity.

If approved by the FDA, sotatercept would be the first therapy that acts directly against the cause of the disease.

Although commercial accountable care organization populations are healthy on average, some individuals might benefit from programs for high-risk patients to mitigate high levels of health care utilization.

Study authors said the findings could inform clinicians when selecting therapies for patients with type 2 diabetes (T2D). However, an editorial found the follow-up period too short and differences between the study arms too small to be meaningful.

Oncology has been an easy area for employers to adopt biosimilars because of the rising costs in the space, said Margaret Rehayem, vice president, National Alliance of Healthcare Purchaser Coalitions. Now that multiple adalimumab (Humira) biosimilars are hitting the US market, employers should take a step back to review their current strategy around the drug.

Rebates remain very attractive for many employers, but they should push back on the reliance on rebates that may be preventing biosimilars from being added to formularies, said Margaret Rehayem, vice president, National Alliance of Healthcare Purchaser Coalitions.

Increases in Medicare Advantage market share over the past 10 years are largely caused by an increased preference for managed care among Medicare beneficiaries.