
Health Care Cost
Latest News
Latest Videos

CME Content
More News

Speakers at Patient-Centered Oncology Care® highlighted injustices in the US health care system, the risk of financial toxicity, and how providers can do a better job to ensure their patients achieve health equity, during a panel discussion.

The survey was released to mark Pain Awareness Month.

A cost-saving provision made possible by the recent COVID-19 relief CARES Act now allows Americans to leverage pre-tax funds from their flexible spending arrangements [FSAs] or health savings accounts [HSAs] to purchase over-the-counter medicines and menstrual care products.

Sickle cell disease is a costly disease for patients, but when those patients suffer from end-organ damage, the costs jump significantly.

A decision-analytic model could save more than $7 million in overall ineffective health care costs per 1000 patients by predicting which patients with rheumatoid arthritis (RA) will have an inadequate response to anti–tumor necrosis factor therapies.

Patients with spinal muscular atrophy (SMA) incur significant health care resource utilization and cost burden, particularly those with infantile-onset SMA.

A review warns against delaying or ignoring the concerns of individuals with chronic pain during the coronavirus disease 2019 (COVID-19) pandemic.

Kidney failure is one of the expensive conditions in health care, but new results from the DAPA-CKD trial could change the equation in favor of prevention.

In this episode of Managed Care Cast, we talk with Michael N. Abrams, a cofounder and managing partner of Numerof & Associates, about the fifth annual report on the state of population health.

In this episode of Managed Care Cast, we share a little bit of our forthcoming interview with Georges C. Benjamin, MD, executive director of the American Public Health Association, which will appear in the September issue of The American Journal of Managed Care®.

Children receiving intensive chemotherapy benefit from prophylaxis with levofloxacin to an extent that would justify the cost of the drug, a new analysis finds.
Current therapeutic options for multiple myeloma and best practices in dispensing medications throughout the COVID-19 pandemic.

Through the partnership between Innovaccer and Emtiro Health, data utilization will work to delineate and address social aspects known to affect the health of populations nationwide, said Kelly Garrison, CEO at Emtiro Health, and Paul Grundy, MD, chief transformation officer at Innovaccer.

The challenges of complying with payer mandates in biosimilars were discussed in a webinar sponsored by The American Journal of Managed Care® and The Center for Biosimilars®.

Given the constraints prevalent post-COVID-19, Dr Mark Fendrick, director of the University of Michigan Center for Value-Based Insurance Design, stresses that it is now more important than ever for the health care industry to prioritize payment reform, value-based benefit design, and novel policy initiatives.

Despite concerns, legislation to cap out-of-pocket payments for specialty drugs has not been shown to shift costs to health plans, thereby increasing insurance premiums, according to a study published in New England Journal of Medicine.
The coronavirus disease 2019 (COVID-19) vaccines that are leading the pack are utilizing a new vaccine technology that has never been approved for human use by the FDA. As a result, there are a lot of unknowns.
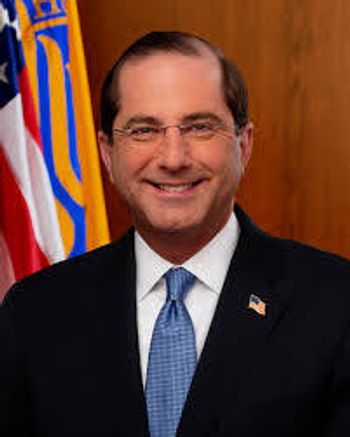
The ruling reversed a lower court ruling regarding the drug discount program for hospitals that serve patients covered by Medicaid.

End-stage renal disease has long been one of the most expensive and debilitating conditions that affects Medicare beneficiaries. Not only does dialysis cost $90,000 a year—those awaiting a kidney transplant automatically qualify for Medicare—but the need to travel to a dialysis center multiple times a week disrupts employment and home life.

Oncology practices could use more time to become accustomed to 2-sided risk even without a global pandemic, but the current crisis makes the need more urgent, say payment reform leaders at the Community Oncology Alliance virtual conference.

At the 2020 Community Oncology Conference, hosted by the Community Oncology Alliance, Howard "Skip" Burris III, MD, FACP, FASCO, president, chief medical officer, and executive director of drug development for Sarah Cannon Research Institute, will discuss "The Now and Future of Clinical Trials in the Community Oncology Setting." The American Journal of Managed Care® recently spoke with Burris, who is wrapping up his term as president of the American Society of Clinical Oncology, about how the coronavirus disease 2019 pandemic is affecting clinical trials as well as other aspects of the future of patient care in community oncology settings.

As Kidney Week closed, nephrologists gathered to hear policy updates and information about forthcoming payment models from CMS and seemed pleased with what they heard.

This article provides an overview of the impact of specialty care and the opportunity for it to leapfrog primary care as a lead focus for accountable care.

This paper presents a method to characterize policy implementation across states to enable more nuanced impact assessments of federal healthcare delivery system and payment reforms.

Physician groups have begun designing alternative payment models for their own specialties, proposing that CMS include financial risk, funding for new technologies, and legal waivers.


















