
Mitigating the high cost of prescription drugs is a win-win to address the complex, multipronged problem of getting patients to take their medications as advised.

Mitigating the high cost of prescription drugs is a win-win to address the complex, multipronged problem of getting patients to take their medications as advised.

New research published in Health Affairs details the rates of specialty medication noninitiation among Medicare Part D beneficiaries.

Norman E. “Ned” Sharpless, MD, is departing shortly after the launch of Cancer Moonshot 2.0, an initiative that aims to reduce the cancer death rate by at least half over the next 25 years while improving the experience for all those affected by cancer.

Conversations are ongoing between CMS and patient advocates on how accountable care organizations (ACOs) and similar programs can better interface with beneficiaries.

Although the medication therapy management program in Tennessee's Medicaid population did not reduce costs, some adherence to medication improved and emergency department visits improved.

The American College of Cardiology will host its annual conference beginning Friday, April 1, 2022, both in-person and online.

President Biden releases the budget for fiscal year 2023; health care spending is projected to hit $6.8 trillion in 2030; rates of prediabetes on the rise in children.

New research found Medicaid expansion was associated with lower rates of diabetic limb amputations among racial minorities in the United States.

The FDA approved a drug to treat a rare form of childhood epilepsy; uninsured Americans will no longer have access to free COVID-19 tests; a conservation group is suing the Environmental Protection Agency (EPA) over failure to protect rivers from pollution.

Angela Storseth-Cooper, associate director, Government Relations & Public Policy, The US Oncology Network, discusses state-level legislation that community oncology practices can leverage to address issues involving pharmacy benefit managers and the vertical integration of health plans and specialty pharmacies.

The World Health Organization warns of long-term health impacts from the Ukraine crisis; states sign legislation aimed at curbing abortion access; over 14 million Americans signed up for health insurance through the Affordable Care Act.
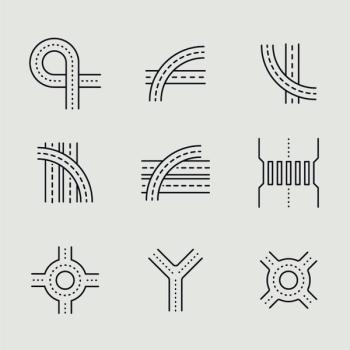
Built environments can shape how active an individual is, while policy decisions made decades ago impact health disparities today. To address these critical social determinants of health, experts are calling for increased cooperation between urban planners and the public health field.

On this episode of Managed Care Cast, Lori Timmins, PhD, and Eugene Rich, MD, discuss the findings of their interim analysis of data from the first 3 years of the Comprehensive Primary Care Plus Initiative, a large-scale effort of primary care redesign meant to improve care fragmentation among Medicare fee-for-service beneficiaries.

A new COVID-19 response coordinator will replace Jeff Zients; cigarette smoking rates were down in 2020; mental health providers offer telehealth services to Ukraine.

This new investigation evaluated outcomes among 6 youths with type 1 diabetes, who had public insurance coverage and received continuous glucose monitoring assistance through the CGM Time in Range Program.

Full approval by the FDA follows tentative approval for the complex drug delivery advice for asthma and chronic obstructive pulmonary disease (COPD) granted by the FDA last week amid a patent dispute.

On this episode of Managed Care Cast, Anna Forsythe, PharmD, MSc, MBA, vice president of value and access at Cytel, explains the monetary and humanistic costs of conversion therapy among LGBTQ+ populations in the United States.

The authors found an association between Medicare’s wage index adjustment and the differential use of labor-intensive surgical procedures and medical device–intensive minimally invasive clinical procedures across the United States.


Medicare beneficiaries attributed to small practices in accountable care organizations (ACOs) achieve greater savings than beneficiaries attributed to large practices in ACOs.

A new opinion indicates paying those with substance use disorder to stay clean could be legal; the 2020 Census undercounted some racial minorities; the true global COVID-19 death toll could be 3 times higher than the official tally.

The growth of 340B contract pharmacies since 2010 is unprecedented. This study’s findings suggest that patterns of growth differ between safety-net clinics and hospitals.

Developing alternative payment models for commercial populations in specialties such as oncology is rife with practical challenges. Leading payers and practices share lessons to date.

An analysis of 2019 claims data for California Medicaid enrollees shows large disparities in HIV pre-exposure prophylaxis (PrEP) uptake, especially among Black individuals.

Natalie Dickson, MD, president and chief strategy officer of Tennessee Oncology, discusses Tennessee Oncology's role in the discussion to reform 340B.

259 Prospect Plains Rd, Bldg H
Cranbury, NJ 08512
© 2025 MJH Life Sciences®
All rights reserved.
