- April 2021
- Volume 27
- Issue 3
AJMCtv Interviews: April 2021
AJMC®TV interviews let you catch up on what’s new and important about changes in healthcare, with insights from key decision makers—from the clinician, to the health plan leader, to the regulator. When every minute in your day matters, AJMC®TV interviews keep you informed. Access the video clips at ajmc.com/interviews. These interviews have been edited lightly for clarity.
Dr Apar Kishor Ganti Explains Why Lurbinectedin Is Important for Patients With SCLC
APAR KISHOR GANTI, MD, IS A PROFESSOR OF INTERNAL MEDICINE IN THE DIVISION OF ONCOLOGY & HEMATOLOGY AT THE UNIVERSITY OF NEBRASKA MEDICAL CENTER.
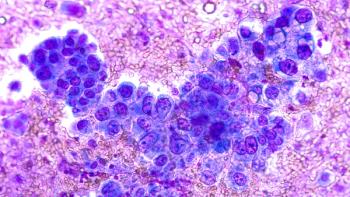
Lurbinectedin is a selective oncogenic transcription inhibitor that is being studied in 9 different tumor types. Can you discuss its mechanism of action? Why does it offers promise for certain patients with small cell lung cancer (SCLC) when a first-line therapy fails?
Kishor: Lurbinectedin inhibits oncogenic transcription. Basically, it prevents the binding of transcription factors to their sequences. Therefore, it prevents transcription, and transcription is what’s responsible for cell division. [Preventing transcription] eventually leads to cell death or apoptosis. In addition to lurbinectedin blocking [transcription] in tumor cells, it also inhibits transcription in the tumor-associated macrophages; therefore, it can affect the tumor
microenvironment as well.
It is important, or [particularly] exciting, because a new trial was published recently in The Lancet in which they looked at lurbinectedin in SCLC. It has been studied in other tumor types as well, but this was a report specifically in SCLC, and in this group of patients, who had previously received at least 1 line of chemotherapy, about 35% of the entire population responded. Historically, in that cohort of patients, response rates range between 15% and 20%. So, when this study reported a 35% response rate, that automatically became pretty big news.
What is the recommendation for lurbinectedin in the National Comprehensive Cancer Network (NCCN) guidelines?
Kishor: NCCN guidelines recommend lurbinectedin in the relapse setting, meaning in patients who have failed at least 1 previous line of chemotherapy. It’s the second drug that has been FDA approved in this setting, after topotecan. The NCCN guidelines recommend that as the preferred option in patients who have failed SCLC [therapy] and for whom more than 3 months have passed since their previous treatment. [In other words, they’ve had a] chemotherapy-free interval of 90 days; for patients with a chemotherapy-free interval of less than 90 days, it is an option.
Dr Ashley Ross on Genomic Testing Post Prostatectomy
ASHLEY ROSS, MD, PHD, IS A UROLOGIST AND ASSOCIATE PROFESSOR AT THE NORTHWESTERN UNIVERSITY FEINBERG SCHOOL OF MEDICINE.
Can you discuss the current treatment landscape for postprostatectomy patients? What are the benefits of utilizing genomic testing to plan the right approach?
Ross: Previously, trials have focused on adjuvant radiation treatment vs just waiting. [Some] trials showed oncologic benefit for giving adjuvant treatment over doing nothing, but the number of men who needed to be treated with therapy was fairly high. More importantly, a lot of those trials looked at adjuvant treatment vs what often was a delayed salvage approach, in which the patients’ prostate-specific antigen (PSA) [measurements] were actually fairly high. Over the last year or so, clinical trials have been published looking at adjuvant therapy vs early salvage therapy.1,2
What those trials showed is that if you have disease that is Gleason grade group 2 or 3, and particularly if you have no seminal vesicle involvement and no lymph node involvement, then an early salvage approach might be favored vs an adjuvant radiation approach. But how about men who don’t [have] those characteristics and who were underrepresented in those trials? Men with Gleason 8 to 10 disease, meaning Gleason grade group 4 or 5, and men with T3b disease, meaning they have disease in the seminal vesicles, were unrepresented in the RADICALS and RAVES trials. And those men still have treatment decisions about whether they should they jump on their cancers early or not. What genomic classifiers do, or genomic information does—particularly the Decipher score—is provide independent prognostic information beyond your clinical pathologic characteristics. Previous retrospective studies have shown that you might be better suited for adjuvant therapy, as opposed to a salvage approach, and potentially even an early salvage approach, if you have a constellation of higher-risk features, at least 2 of the following: Gleason 8 to 10; T3b disease; or a high genomic classifier score, meaning a Decipher score higher than 0.60. That’s going to be fleshed out in prospective clinical trials. But right now, that’s a sweet spot for genomics. You can help decide: Are you going to use this therapy or not? Let’s pretend that you waited until your [patient’s] PSA started to rise—and particularly now with ultrasensitive PSA checks, a lot of us are doing that, waiting until the PSA gets to some low level—but let’s pretend that it’s even 0.10. And now you’re deciding, based on the clinical trials have been published, that you do want to give a salvage therapeutic approach. The questions that appear now are: Should that salvage therapy be alone, or should it be [in conjunction] with hormonal therapy? A previous trial, RTOG 9601, showed that in the salvage radiation setting, adding 2 years of hormonal therapy—in that trial, they used bicalutamide for 2 years—would improve oncologic outcomes.3
However, that trial included many men with higher PSA levels, and a subset analysis of men with lower PSAs showed that adding on the bicalutamide might be an overall detriment to survival if you’re radiating people at low PSAs.4 So here’s another place where the molecular testing really can shine and help you with your clinical decision-making.
A paper in press looks at RTOG 9601 and a subset of the men who had testing with the genomic classifier. It showed that adding hormonal therapy would actually cause an overall survival detriment for men at low genomic risk and who had low PSA. [This] tells us to avoid hormonal therapy if you’re going to do salvage radiation in those men, particularly early salvage radiation. On the flip side, you may want to intensify with hormonal therapy, if they have a high genomic risk and you’re doing even early salvage radiation. So, [genomic testing] is giving you important prognostic information in addition to your clinical information about whether or not you should do salvage radiation therapy, and [if so,] how intense you should make that.
References
1. Parker CC, Clarke NW, Cook AD, et al. Timing of radiotherapy after radical prostatectomy (RADICALS-RT): a randomised, controlled phase 3 trial. Lancet. 2020;396(10260):1413-1421. doi:10.1016/S0140-6736(20)31553-1
2. Kneebone A, Fraser-Browne C, Duchesne GM, et al. Adjuvant radiotherapy versus early salvage radiotherapy following radical prostatectomy (TROG 08.03/ANZUP RAVES): a randomised, controlled, phase 3, non-inferiority trial. Lancet Oncol. 2020;21(10):1331-1340. doi:10.1016/S1470-2045(20)30456-3
3. Shipley WU, Seiferheld W, Lukka HR, et al; NRG Oncology RTOG. Radiation with or without antiandrogen therapy in recurrent prostate cancer. N Engl J Med. 2017;367(5):417-428. doi:10.1056/NEJMoa1607529
4. Spratt DE, Dess RT, Efstathiou JA, et al. Two years of anti-androgen treatment increases other-cause mortality in men receiving early salvage radiotherapy: a secondary analysis of the NRG Oncology/RTOG 9601 randomized phase III trial. Presented at: 2019 American Society for Radiation Oncology Annual Meeting; September 15-18, 2019; Chicago, IL. Abstract LBA1.
Dr Sibel Blau Discusses the Impact of Delayed Cancer Diagnoses on Community Cancer Practices
SIBEL BLAU, MD, IS A MEDICAL ONCOLOGIST AT NORTHWEST MEDICAL SPECIALTIES, AND PRESIDENT AND CEO OF THE QUALITY CANCER CARE ALLIANCE (QCCA).
Many cancer diagnoses were delayed in 2020, as was much cancer care. How will community cancer practices be impacted when they start to see more patients than
usual diagnosed with a later-stage cancer?
Blau: [The Community Oncology Alliance] published a paper about delay in cancer care and how screening and certain surgeries were put on hold. We started thinking about this [early on,] as the pandemic came to Seattle first [and my practice is in Washington State]. In our practice, we started taking precautions earlier on, and we talked to all our QCCA practices about this. We were in a survival mode, and we tried to see anybody we could, [meaning] we tried not to delay appointments and we tried to utilize telehealth. But as [big of an] advocate as I am for telehealth, it’s just not enough. There has been a true delay in diagnosing those patients with cancer and now, possibly, these patients are going to be coming in later stages.
When you look at health economics, there are actually [thorough] statistics and data coming out on how this is going to affect the economy—not only gross domestic product, but cancer care and health care economy. The cost and burden will be tremendous on physicians, personnel, and practices—[whether] big institutions or smaller practices. We’ll probably see lower access to care, because patients will not be able to get in to see doctors in a timely manner—that will become a big hurdle. Certainly, as QCCA practices, we have regular meetings about [the pandemic], and we discuss these issues, among others, and try to learn from and get tips from each other.
Smaller practices like ours in cancer care are much more nimble, and we can make faster decisions and adapt maybe somewhat more easily. But that doesn’t address the question when the numbers start coming in. I don’t know how we’re going to handle this completely. Also, I think [the picture will vary across the country] from region to region. Some regions did not get affected as much as others by the pandemic, and some centers did not see as much drop in volume as others.
Dr Whitney Goldsberry on the Future of PARP Inhibitors in Ovarian Cancer
WHITNEY GOLDSBERRY, MD, IS A CLINICIAN AT THE UNIVERSITY OF ALABAMA AT BIRMINGHAM HOSPITAL AND A FELLOW IN THE UAB DIVISION OF GYNECOLOGIC ONCOLOGY.
PARP inhibitors have seen several new indications since they were first approved for ovarian cancer treatment in 2014. What trends did you see in cost over time?
Goldsberry: Although our study1 was limited by a small number [of patients], we did note a few general patterns. The overall monthly cost of PARP inhibitors appeared
to actually decrease from 2017 to 2019. Similarly, the monthly costs covered by payers appeared to decrease slightly, reflecting a decrease in the overall cost. Through this, thankfully, the out-of-pocket cost actually remained very low. We did notice that the contribution of financial assistance programs did increase over time, which may reflect improved utilization of existing financial assistance programs. These trends will be very important as we move forward in the broader applications of these drugs.
What do you see on the horizon for PARP inhibitors in ovarian cancer treatment, whether in novel therapies/combinations or in regulatory changes?
Goldsberry: I think the next steps in PARP inhibitor development include identifying additional biomarkers that may indicate which patients will benefit the most from this class of therapies. Currently several clinical trials are looking into combining PARP inhibitors with other types of therapies, such as immunotherapy or other antiangiogenics, to see if these combinations have a synergistic effect. It’ll also be interesting to see the efficacy of PARP inhibitors used after prior PARP inhibitor [therapy]. Inevitably, more information will [emerge] on this topic as we start to increase PARP inhibitor use in frontline treatment.
Reference
1. Goldsberry WN, Summerlin SS, Guyton A, et al. The financial burden of PARP inhibitors on patients, payors, and financial assistance programs: who bears the cost? Gynecol Oncol. Published online January 4, 2021. doi:10.1016/j.ygyno.2020.12.039
Articles in this issue
almost 5 years ago
Path to Better Payment System to Be Clear Over Timealmost 5 years ago
Medical World News: Clinical, Regulatory, and Managed Care Updatesalmost 5 years ago
Conference Coverage: Association of Community Cancer Centers 2021almost 5 years ago
Disparities in Cancer Care: Has Precision Medicine Widened the Gap?almost 5 years ago
The Impact of Reinsurance of Gene Therapies on Employer Financial RiskNewsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.