Canadian Study Explores Use of Liquid Biopsies in Advanced NSCLC
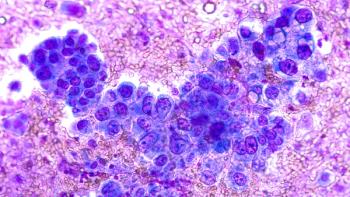
Next-generation sequencing (NGS) of cell-free DNA (cfDNA) may improve diagnostic testing in advanced lung cancer.
Next-generation sequencing (NGS) of cell-free DNA (cfDNA) obtained from blood samples may improve
The research was published as part of the IASLC 2020 Lung Cancer Hot Topic: Liquid Biopsy Virtual Conference. A
The study, involving 210 patients in 2 cohorts, took place at 6 Canadian hospitals.
Cohort 1 included 150 treatment-naïve patients with measurable disease and smoking history of fewer than 10 packs of cigarettes per year. Cohort 2 enrolled 60 patients with known oncogenic drivers whose disease progressed on tyrosine kinase inhibitors (TKIs).
After excluding variants of unknown significance and synonymous alterations, 118 patients in cohort 1 (79%) had more than 1 alteration detected by G360 test (304 alterations detected in 35 genes). Of these, 284 alterations were considered actionable with FDA-approved drugs or available clinical trials.
Actionable targets included EGFR (32.0%), ERBB2 (3.2%), MET (3.2%), ALK (1.4%), KRAS G12C (1.1%), and ROS1 (0.4%). Additional clinically relevant alterations included TP53 (27.8%), KRAS non-G12C (3.9%), PIK3CA (3.9%) and BRAF nonV600E (1.1%).
In cohort 2, 53 patients (85%) had more than 1 characterized genomic alteration detected, with a total of 165 alterations in 28 genes including EGFR (45.8%, 5 were C797S), ALK (fusions 3.3%; mutations 2.0%), BRAF (V600E 0.7%; other 3.3%), MET (amplification 2.0%; exon 14 0.7%), FGFR3 (0.7%), and RET (0.7%) as well as non-driver mutations.
Twenty-seven patients (14.0% in cohort 1; 10% in cohort 2) had no alterations detected by G360. In samples with alterations detected, the median number of alterations per patient was 3 (range 1-17). The median time to reporting of G360 was 7 days (range 5-27).
The idea of using blood biopsies first is growing as it may be faster, less expensive, and more specific compared with standard tissue profiling.
"Over 80% of patients with advanced NSCLC had characterized genomic alterations detected in cfDNA. At least 56% of treatment-naïve patients and 37% of TKI-resistant patients had clinically actionable alterations detected," said study lead by Natasha Leighl, MD, Princess Margaret Cancer Centre, Toronto, Canada,
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.