In Study Across 15 Centers, 35% of Patients With MCL See Progression After CAR T-Cell Therapy
Key Takeaways
- Approximately one-third of patients with relapsed or refractory mantle cell lymphoma (MCL) in this study treated with CAR T-cell therapy experienced disease progression, with a median progression time of 6 months.
- Brexucabtagene autoleucel and lisocabtagene maraleucel, FDA-approved CAR T-cell therapies, show high response rates but are not curative for MCL.
Study reveals one-third of mantle cell lymphoma patients in a study at leading cancer centers experienced disease progression after CAR T-cell therapy, highlighting treatment challenges and outcomes.
About a third of patients with relapsed or refractory (R/R) mantle cell lymphoma (MCL) who are treated with chimeric antigen receptor (CAR) T-cell therapy see their disease progress, according to a study of 384 patients from 15 international cancer centers.1
The study appeared August 5 in Blood Advances, a publication of the American Society of Hematology.1
Investigators from leading centers, including Memorial Sloan Kettering (MSK), The University of Texas MD Anderson, and Mayo Clinic, published results this month in Blood Advances,1 exploring common factors among the 135 patients with disease progression following CAR T. The median time to progression was 6 months.
FDA has approved 2
The authors report that brexu-cel is associated with an overall response rate (ORR) of 91% and a median progression-free survival (PFS) of 25.8 months; liso-cel is associated with an ORR of 83% and a median PFS of 15.3 months. Neither is considered curative.
Median follow-up for all patients with MCL receiving CAR T-cell therapy, including those not experiencing disease progression at the time of data cutoff, was 25 months. Among the 135 patients who had disease progression, data reported by the investigators is as follows:
- Patients progressing were 74% male, with median 67 years of age (interquartile range, 61-72).
- 98% received at BTK inhibitor before CAR T-cell therapy, with 63% having a response.
- Median lines of therapy before leukapheresis were 3 (range, 1-9).
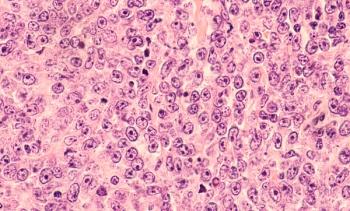
- High-risk features prior to CAR T-cell therapy were common and included: 68% with TP53 mutation, 69% with Ki67 at least 50%; 16% with central nervous system (CNS) involvement, and 25% with blastoid/pleomorphic MCL.
- Most patients who eventually progress had bridging therapy (73% ), and 60% whose responses were assessed were refractory to bridging.
- Patients received brexu-cel (87%) or liso-cel (13%) at physician’s choice, predominantly with fludarabine/cyclophosphamide lymphodepletion (87%).
Following treatment, 64% of these same patients had a complete response (CR), with 27% having a partial response (PR) and 16% having stable disease. Other features of these patients included:
- Median time from CAR-T infusion to disease progression was 6 months (interquartile range, 3-11) and only 30 patients experienced disease progression more than12 months following CAR-T infusion.
- At the time of disease progression, high-risk MCL features included 28/78 (37% (37%) with blastoid/pleomorphic morphology; 50/65 (77%) with Ki67 of at least 50%, and 21/41 (51%) TP53-mutated MCL; 11 of 22 patients with CNS disease prior to CAR-T had CNS involvement at disease progression.
- There were 79 patients whose CD19 status was assessed with a biopsy following disease progression, and 10% had CD-19 negative disease.
Following disease progression, 17 patients had no further treatment. Another 13 received local therapy, and 105 received systemic therapy. The most common therapies following CAR-T included:
- chemoimmunotherapy, 22 patients, ORR 40%
- pirtobrutinib, 17 patients, ORR 36%
- bispecific antibodies, 13 patients, ORR 67%.
For patients experiencing disease progression, the median PFS and overall survival (OS) were 2.5 months and 5.4 months, respectively. Lack of response to CAR-T and a short time from CAR-T infusion to progression (less than 3 months vs 3-6 months vs more than 6 months), were among the factors associated with inferior OS.
“In conclusion,” the authors wrote, “We confirm the challenging prognosis for patients experiencing [disease progression] following CD19 CAR-T for R/R MCL and establish a benchmark for future.”
References
- Epstein-Peterson ZD, Lionel AC, Joseph A, et al. Treatment and outcomes of progression of disease post-CAR T-cell therapy in mantle cell lymphoma: a multicenter analysis. Blood Adv. Published August 5, 2025.
doi.org/10.1182/bloodadvances.2025016315 - Stallard J. FDA approves CAR T cell treatment for resistant mantle cell lymphoma. Memorial Sloan Kettering Cancer Center. July 31, 2024. Accessed August 15, 2025.
https://www.mskcc.org/news/fda-approves-car-t-cell-treatment-for-resistant-mantle-cell-lymphoma
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.