News
Article
Recombinant Hirudin May Help Treat Diffuse Large B-Cell Lymphoma
Author(s):
Recombinant Hirudin (rH) inhibited the polarization of M2-type macrophages and protease-activated receptor-1 (PAR-1) in diffuse large B-cell lymphoma (DLBCL).
A study of 32 clinical samples from patients with diffuse large B-cell lymphoma (DLBCL) found that recombinant Hirudin (rH) curbed the polarization of M2 macrophages, and that protease-activated receptor-1 (PAR-1) regulated cell proliferation, migration, invasion and angiogenesis, according to a proof-of-concept study based in China and published in BMC Biotechnology.1
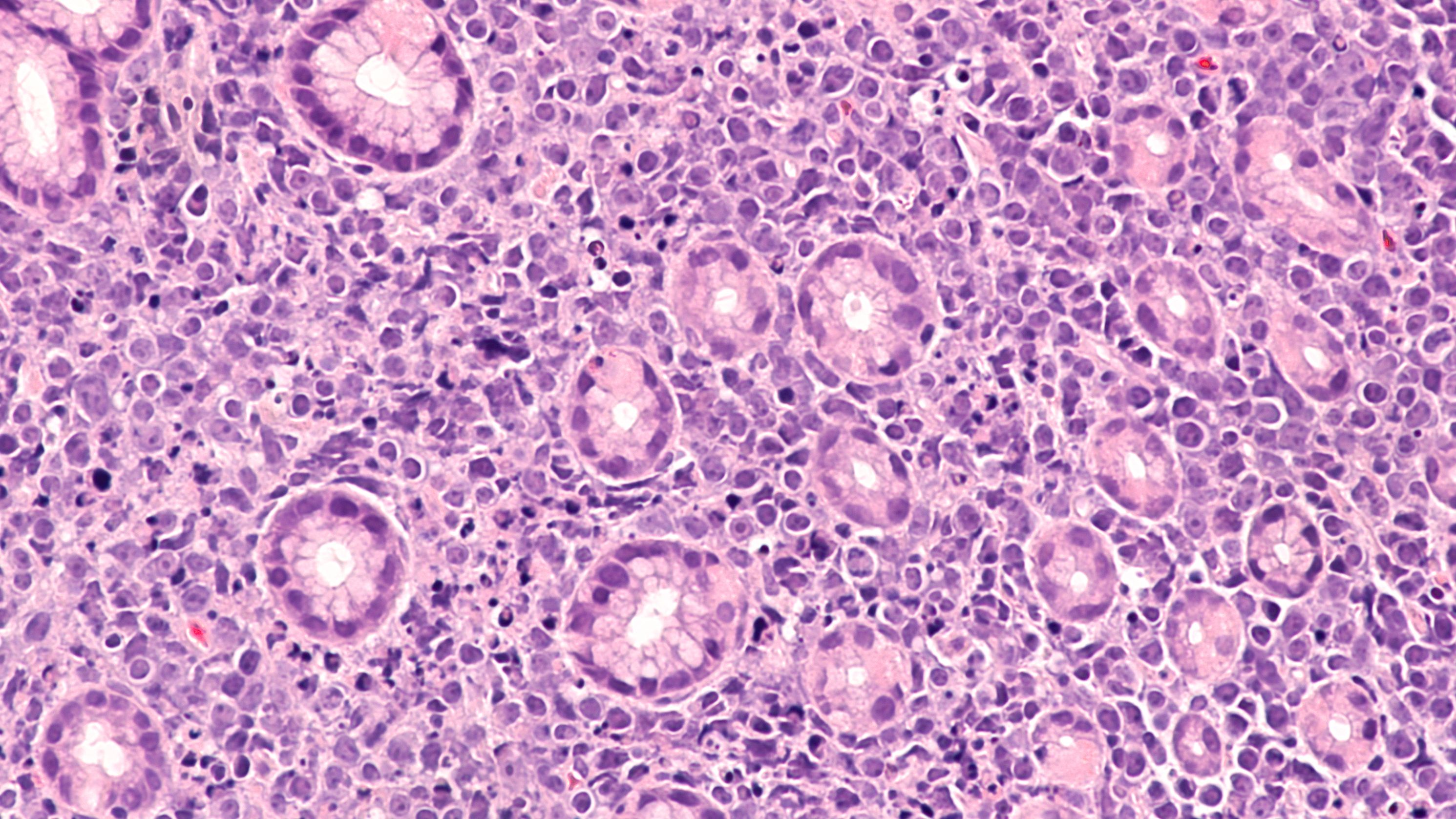
Recombinant Hirudin shows promise in the treament of DLBCL | image credit: David A Litman - stock.adobe.com
“Although some standard therapies have been established to improve the cure rate [of DLBCL], they remain ineffective for specific individuals. Therefore, it is meaningful to find more novel therapeutic approaches,” the authors wrote. “Macrophage polarization is extensively involved in the process of tumor development. Recombinant hirudin (rH) affects macrophages and has been researched frequently in clinical trials lately. Our article validated the regulatory role of rH in macrophage polarization and the mechanism of PAR-1 by collecting clinical samples and subsequently establishing a cellular model to provide a scientifically supported perspective for discovering new therapeutic approaches.”
Researchers first evaluated cell polarization and expression of validation cytokines through flow cytometry, ELISA, and RT-qPCR to confirm the success of the cell model, which was co-cultured with THP-1 and OCI-L10 lymphoma cells.1 They examined CD68 + pSTAT1 + cells (M1 macrophages) and CD163 + CMAF + cells (M2 macrophages) in diseased and nearby tissues, finding higher expression of M2 macrophage and PAR-1 markers in the cell model, which was consistent with the clinical samples.
Researchers then added varying doses of rH and discovered that PAR-1 regulated cell proliferation, migration, invasion and angiogenesis of DLBCL-associated macrophages. Flow cytometry analysis showed that the positive rate of M1 macrophages decreased significantly in disease samples, while M2 macrophages increased significantly. Researchers used RT-qPCR to detect the cytokines and detected reduced expression of interleukin-6 (IL-6), tumor necrosis factor (TNF)-α and IL-1β and increased expression of IL-10, TGF-β and Arginase (Arg).
The study also found that PAR-1 promotes the conversion of M2 macrophages to M1 macrophages.
Microphages are a type of white blood cell that kills microorganisms, removes dead cells, and triggers the action of other immune system cells, according to the National Cancer Institute.2
They are derived from mononuclear phagocytes, which possess strong heterogeneity and plasticity. Microphages can affect immune regulation, and exhibit polarization, or various activation states in response to changes in the microenvironment. Macrophages are divided into two states, M1 (classically activated) and M2 (alternatively activated). M1 macrophage activation describes an adaptive immune response in which pro-inflammatory cytokines are released, such as Th1 cytokines tumor necrosis factor TNF-α, IL-6 and IL-1β. M2 macrophages release the anti-inflammatory factors IL-10, TGF-β and Arg, which leads to wound healing.
An imbalance between M1 and M2 has been proven to be a factor that leads to cancer, cardiovascular diseases, liver diseases and neurodegeneration. Previous research has linked macrophages with poor cancer prognosis, the authors stated.
Overexpression of PAR-1, a promising molecular target in cancer, leads to higher invasive and migratory capacity in cancer cells and is associated with distal metastasis of cancer cells in various cancer cell lines. PAR-1 is associated with angiogenesis and vascular endothelial growth factor levels, according to the study.
“Patients who receive rituximab treatment have an overall survival rate of approximately 65% in five years. Despite the ability of this chemotherapy modality to improve patient prognosis, abnormalities in the tumor microenvironment continue to influence the progression of DLBCL,” the authors wrote. “Our findings may provide a basis for the therapeutic role of hirudin in DLBCL.”
References
- Pei Q, Li Z, Zhao J, Zhang H, Qin T, Zhao J. Recombinant hirudin and PAR-1 regulate macrophage polarisation status in diffuse large B-cell lymphoma. BMC Biotechnol. 2024;24(1):55. doi:10.1186/s12896-024-00879-w
- Macrophage. National Cancer Institute. Accessed August 29, 2024. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/macrophage
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.




