Vaccine Plus Pembrolizumab Shows Promise in Breast Cancer in Animal Study
The study, using mice, also found that the 2-step therapy was more effective the earlier it was given.
Pembrolizumab administered in conjunction with an investigational vaccine showed promise for tumor reduction and long-term survival in mice with HER2-positive breast cancers, according to study results released this week.
The study, by researchers at the Duke Cancer Institute, was published in Clinical Cancer Research. The targeted
The current preclinical study also found that the 2-step therapy was more effective the earlier it was given. This could have future implications for trials, which normally enroll patients with more advanced disease.
HER2-positive breast cancers are responsible for about 20% of all breast cancers.
The Duke-created vaccine specifically targets HER2Δ16, an oncogenic driver and cause for resistance to HER2-positive breast cancer. It makes up about 10% of HER2 transcripts.
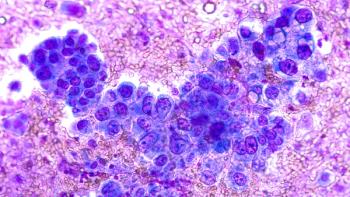
The vaccine plus pembrolizumab incites CD8 T-cells, resulting in pronounced tumor reduction and long-term tumor-free survival.
Pembrolizumab, sold as Keytruda by Merck, increases the ability of the body’s immune system to help detect and fight tumor cells by blocking the interaction between programmed cell death protein 1 (PD-1) and its ligands, PD-L1 and PD-L2. This activates T lymphocytes which can affect both tumor and healthy cells. Due to the high number of mutations present in TMB-H tumors, they are easier for the immune system to identify, and thus may be more likely to respond to certain immunotherapies.
Used alone, pembrolizumab has shown limited effect on HER2-positive breast cancers. In this study, the researchers found that vaccine-induced HER2-specific T-cells were essential for a sustained immune response.
"The basic premise is that the immune checkpoint inhibitors work fantastic if the body has already triggered an immune response, but they don't work well in the absence of that," H. Kim Lyerly, MD, a professor in the departments of Surgery, Immunology and Pathology at Duke University School of Medicine and an author of this study,
Reference
Crosby EJ, Acharya CR, Haddad A, et al. Stimulation of oncogene-specific tumor infiltrating T-cells through combined vaccine and αPD1 enable sustained anti-tumor responses against established HER2 BC. Clin Cancer Res. Published online July 30, 2020. Doi: 10.1158/1078-0432.CCR-20-0389
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.