
Patients with blood cancers are burdened with higher costs than patients with other cancers, and spending in blood cancers does not return to precancer levels, according to a new study from the Leukemia & Lymphoma Society.

Laura Joszt, MA, is the vice president of content for the managed care and pharmacy brands at MJH Life Sciences®, which includes The American Journal of Managed Care®, Managed Healthcare Executive®, Pharmacy Times®, and Drug Topics®. She has been with MJH Life Sciences since 2011.
Laura has an MA in business and economic reporting from New York University. You can connect with Laura on LinkedIn or Twitter.

Patients with blood cancers are burdened with higher costs than patients with other cancers, and spending in blood cancers does not return to precancer levels, according to a new study from the Leukemia & Lymphoma Society.

Data and collaboration are necessary ingredients to succeed in the transition to value-based care models, and the money saved under these models will create room to pay for unconventional therapies and services in healthcare, according to panelists at The Institute for Value-Based Medicine meeting in Seattle, Washington.

Progress in health around the globe has stagnated in some countries and gotten worse in others as the world faced increases in conflict and terrorism, epidemics, and noncommunicable diseases, according to global disease estimates published in The Lancet.

In addition to voting for representatives whom people thought would align with their healthcare views, voters in multiple states were faced with ballot measures related to healthcare on November 6. Here are 5 healthcare ballot measures and how they fared in the 2018 midterm elections.
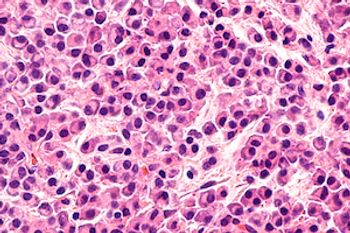
Daratumumab, a human CD38-directed monoclonal antibody, has been confirmed as safe in a population of heavily pretreated patients with multiple myeloma who received access to the treatment before the medication was commercially available, according to an early access treatment protocol study published in Cancer.

Effective care coordination can improve health outcomes for patients with chronic conditions, and a new study found that partnering such a model with bundled interventions can lower spending, as well as improve outcomes, for patients in an urban environment.

While survival from leukemia improved among adults from 1995 to 2009, and the survival gap between sexes decreased, the racial gap did not, according to new research published in Cancer.

New guidelines released by the American Academy of Dermatology will help physicians provide the best treatment for more than 1 million Americans living with melanoma, the deadliest form of skin cancer. The guidelines also highlight the importance of discussions between physicians and patients.

Oregon has approved new policies to continue the transformation of its Medicaid program with a focus on behavioral health, value, and social determinants of health in the state's coordinated care organizations.
In the last decade, testing for and treatment of chronic lymphocytic leukemia (CLL) had undergone substantial changes with new testing that can personalize therapy and new agents that provide more clinical benefit.

Lalan Wilfong, MD, moderated a conversation between Robert E. Baird, MD, CEO of Dayton Physicians Network, and Sarah Cevallos, chief revenue cycle officer for Florida Cancer Specialists and Research Institute, about current and future strategies for Oncology Care Model (OCM) participation, as well as key lessons from the OCM and how they can be applied in other reform models.

A report from RAND Corporation and the American Medical Association (AMA) describes how alternative payment models (APMs) are affecting multiple aspects of physician practice and offers guidance for efforts to improve APMs and help practices succeed in them.

President Donald Trump unveiled the latest steps his administration is taking to help Medicare drive down the costs of prescription drugs with a plan to allow CMS to determine the price it pays for certain drugs based on the prices that other countries pay.

Speakers at the National Committee for Quality Assurance’s Quality Talks meeting discussed challenges to improving healthcare delivery, such as changing behaviors, moving care outside of institutions, and rebuilding trust among marginalized populations.

Approximately one-third of all US healthcare payments in 2017 were tied to alternative payment models, with the remaining still tied to fee for service. The findings of the Health Care Payment Learning and Action Network report highlighted that even as payments move to value-based models, more spending in models with risk is needed.

Accountable care organizations (ACOs) in the Medicare Shared Savings Program vary considerably in how they treat men with newly diagnosed prostate cancer, according to a study that assessed whether the level of engagement in ACOs by urologists could affect rates of treatment, overtreatment, and spending in prostate cancer care.

The EVI1 gene may be single-handedly at fault for acute myeloid leukemia, according to research published in Nature Communications.

AJMC®TV interviews let you catch up on what’s new and important about changes in healthcare, with insights from key decision makers—from the clinician, to the health plan leader, to the regulator. When every minute in your day matters,AJMC®TV interviews keep you informed. Access the video clips at ajmc.com/interviews.

While mental health diagnosis can be associated with an increased use of emergency department (ED) visits, prior patient visit patterns were also associated with higher future ED use.

An event hosted by the American Enterprise Institute highlighted companies in the private sector that are working on novel ways to transform healthcare and bring better value to patients.



Piecemeal solutions to implement value-based payment arrangements will not be able to effectively enact change. Authors in The New England Journal of Medicine argue that a range of complementary solutions need to be pursued simultaneously based on previously successful tactics on a smaller scale.

Multiple myeloma (MM) occurs 2 to 3 times more frequently in Americans of African descent than in Americans of European descent, and a new study has identified 3 gene types that account for this disparity.

Accountable care organizations (ACOs) have not had a significant impact on cancer care costs and utilization. While cancer care costs did decline from before the introduction of ACOs to after, there was no significant difference in spending decreases between ACO practices and non-ACO practices caring for patients with cancer.

Practices in the US Oncology Network received an average positive payment adjustment under the Merit-based Incentive Payment System (MIPS) of 1.90% for performance in 2017, and 99% of the Network’s physicians were in the top tier of performers. The maximum allowable adjustment is 2.02%. The adjustment based on a clinician’s performance in 2017 impacts the clinician's Medicare reimbursement for 2019.

Although patients have the right of access to their protected health information, actual access remains limited. A new study, published in JAMA Network Open, has found that the processing of requesting medical records remains burdensome despite policy efforts.

Tisagenlecleucel's high price is aligned with the benefit the chimeric antigen receptor T-cell therapy provides over a patient's life. Approximately 40% of patients treated are expected to be long-term survivors.

During the opening plenary and panel at the fall 2018 meeting of the National Association of ACOs (NAACOS), Adam Boehler, of the Center for Medicare and Medicaid Innovation, highlighted the fact that CMS has to provide predictability and simplicity to get more accountable care organizations to take on risk and succeed, but that those who are not "cutting it" should "get out of the way" for others.

The type of cancer a provider treats can determine how well he or she performs under the Oncology Care Model (OCM), according to research from Avalere Health that was presented at the American Society of Clinical Oncology Quality Care Symposium.

259 Prospect Plains Rd, Bldg H
Cranbury, NJ 08512
© 2025 MJH Life Sciences®
All rights reserved.
