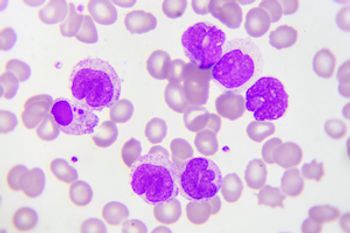
Two abstracts presented at the International Society of Pharmacoeconomic and Outcomes Research Annual International Meeting highlighted patient experiences in blood cancers. One highlighted the worries of patients with acute myeloid leukemia, and the other analyzed economic burdens and resource utilization for patients with non-Hodgkin lymphoma.