
During ESMO Congress 2024, sessions will focus on hot topics in therapeutic areas, such as antibody-drug conjugates; the latest trial data; health policy; and advances in technology.

Laura Joszt, MA, is the vice president of content for the managed care and pharmacy brands at MJH Life Sciences®, which includes The American Journal of Managed Care®, Managed Healthcare Executive®, Pharmacy Times®, and Drug Topics®. She has been with MJH Life Sciences since 2011.
Laura has an MA in business and economic reporting from New York University. You can connect with Laura on LinkedIn or Twitter.

During ESMO Congress 2024, sessions will focus on hot topics in therapeutic areas, such as antibody-drug conjugates; the latest trial data; health policy; and advances in technology.

The transition to value-based care is extremely challenging because everyone is also still being paid by fee for service, said Lalan Wilfong, MD, senior vice president, value-based care, Thyme Care.

There are concerns that the negotiated drug prices under the Inflation Reduction Act (IRA) are leading to large provider reimbursement cuts, explained Nick Ferreyros, managing director, Community Oncology Alliance.

As the pharmacist’s role has evolved in the last decade, they’ve become an important part of reducing costs and better managing patients, explained Scott Soefje, PharmD, MBA, BCOP, FCCP, FHOPA, assistant professor, Mayo Clinic College of Medicines and Science.

The rates of discontinuation due to inefficacy or adverse events for biosimilars and originators of etanercept and adalimumab were similar, according to an analysis of a prospective registry.

A heart failure program with a multidisciplinary team provides statistically significant improvements, and 2 countries determine the current prices of semaglutide are not cost-effective for secondary prevention of cardiovascular disease in patients with obesity, according to abstracts at the European Society of Cardiology (ESC) Congress 2024.

Despite lacking some data, there is some information on which patients with cancer shouldn’t be recommended cannabis or certain cannabis products, said Marie Parish, PharmD, BCOP, a gastrointestinal oncology pharmacist with Mayo Clinic.

Advances in technology have made active surveillance in men with prostate cancer possible and prevented treatment for men who don’t need it, said Matthew Nielsen, MD, FACS, chair, Department of Urology, University of North Carolina School of Medicine.

Research at the European Society of Cardiology Congress 2024 evaluated lipid-lowering therapy beyond statins alone in patients with high levels of low-density lipoprotein cholesterol.

Regardless of duration of type 2 diabetes, sodium-glucose cotransporter inhibitors prevented cardiovascular events, according to research presented at the European Society of Cardiology Congress 2024.

Patients on specialty medications may face many barriers that prevent them from getting on or staying on therapy, but a specialty pharmacy integrated into a health system can help address these issues, explained Ryan Nix, PharmD, MMHC, of Vanderbilt Specialty Pharmacy.

Not all patients will want to take triplet therapy, but those with high-volume prostate cancer who are chemotherapy eligible are usually a good fit, explained Neal D. Shore, MD, FACS.

National data sets and registries are able to provide outcomes data and process measures that testify to quality of care being delivered, said Matthew Nielsen, MD, FACS, chair, Department of Urology, University of North Carolina School of Medicine.

Patients with cancer will never completely replace existing pain regimens, but cannabis could be used in conjunction, explained Marie Parish, PharmD, BCOP, a gastrointestinal oncology pharmacist with Mayo Clinic.

The 10th annual meeting of the Family Heart Global Summit will bring together leading scientists and practitioners with patients to discuss treatment of inherited lipid disorders.

The gene therapy giroctocogene fitelparvovec demonstrated superiority compared with the standard of care, routine prophylaxis, in hemophilia A treatment.





Over the course of the pandemic, the risk of developing long COVID after a COVID-19 infection decreased, largely due to vaccination.

Beneficiaries who switched from traditional Medicare to a Medicare Advantage plan experienced no additional protection from medical costs compared with those who stayed in a traditional Medicare plan.
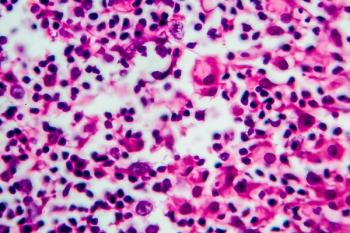
The treatment regimen not only significantly improved progression-free survival (PFS) for patients with advanced stage classic Hodgkin lymphoma but was also better tolerated compared with a 20-year-old regimen being used.

Coverage from the Institute for Value-Based Medicine.

The results of the 3-year follow-up show meaningful improvement in overall survival (OS) and progression-free survival (PFS) for tislelizumab plus chemotherapy compared with placebo plus chemotherapy.

The number of Americans with type 2 diabetes and/or obesity is rising, and the entry of therapies such as glucagon-like peptide-1 (GLP-1) receptor agonists has been revolutionary.

The latest approval of lisocabtagene maraleucel (liso-cel) in mantle cell lymphoma provides another treatment option and continues the tremendous advances in treatment for patients, said Christopher Flowers, MD, of MD Anderson Cancer Center.

The findings can help reduce barriers that delay the onset of recommended palliative care in advanced cancer.

A new program from Optum Rx would offer greater predictability by using a guarantee-based pricing model.

The FDA has approved tarlatamab (Imdelltra; Amgen), a novel bispecific T-cell engager, to treat patients with extensive-stage small cell lung cancer (SCLC).

259 Prospect Plains Rd, Bldg H
Cranbury, NJ 08512
© 2025 MJH Life Sciences®
All rights reserved.
