Oncology
Latest News
Latest Videos

Shorts






Podcasts
More News

Explore the complexities of modern oncology, including precision medicine, CAR T-cell therapies, and challenges in breast cancer care and payer friction.

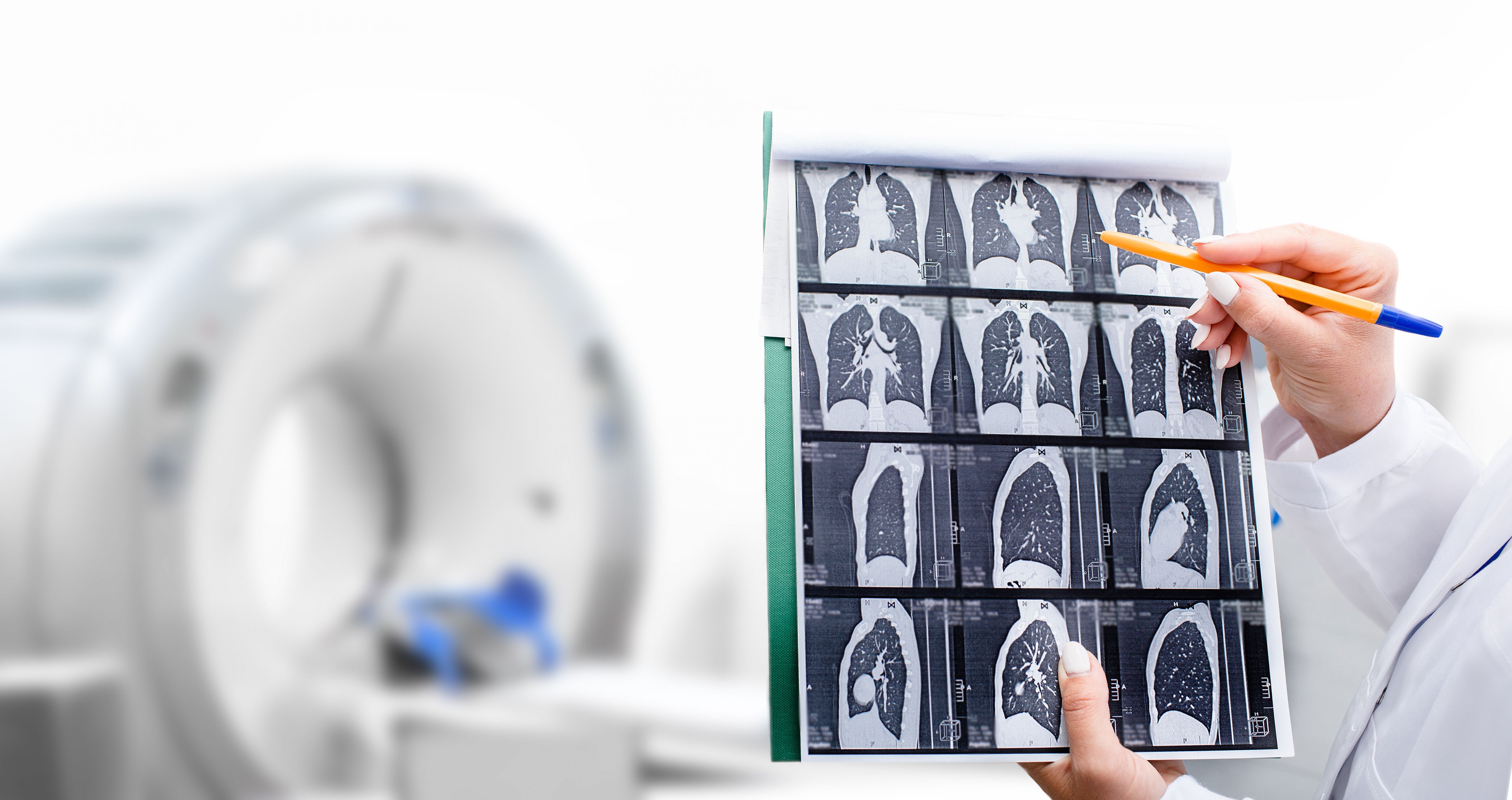
This meta-analysis, which found no statistically significant OS differences by sex, age, or race with ICIs, highlights the need for more diverse, representative NSCLC trials.

Young adults with metastatic CRC (mCRC) and low socioeconomic status (SES) face higher 3-year mortality, whereas race was not independently linked with survival.

Patients with proinflammatory, pro-oxidative diets may face accelerated biological aging and increased skin cancer risk.

Based on these findings, the investigators encourage further research into this promising combination.

Asian women with breast cancer receiving chemotherapy had the highest persistent chemotherapy-induced alopecia (PCIA) incidence and alopecia-related distress vs their White, Black, and Hispanic or Latino peers.

Reader favorites from the 2025 Patient-Centered Oncology Care conference included articles and interviews featuring AI's role in precision medicine and the importance of collaboration in delivering care.

From home-based monitoring and subcutaneous immunotherapy to expanded community cancer networks, 2025 marked a pivotal year in rethinking how cancer care is delivered.

A recent review suggests women with ovarian or colorectal cancer face a higher risk of developing the other, highlighting the need for surveillance.

The foundation of medically integrated pharmacy includes 7 critical pillars. This commentary focuses on the benefits of 3 of those pillars: abandonment, adherence, and access/affordability.

Linvoseltamab shows promise as a first-line therapy for multiple myeloma, offering high response rates and a simplified treatment approach.
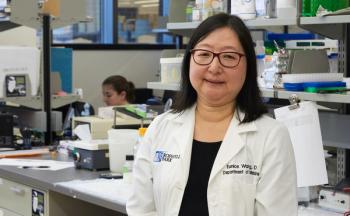
Eunice Wang, MD, highlights breakthroughs in menin inhibitors for acute leukemias, showcasing promising combination therapies and addressing treatment challenges at ASH 2025.

Five key oncology FDA approvals came through last month, expanding treatment options across multiple cancer types.

This approval makes durvalumab with FLOT chemotherapy the first perioperative immunotherapy for resectable gastric or gastroesophageal junction adenocarcinoma.

The FDA approved selumetinib for adults with neurofibromatosis type 1 and symptomatic, inoperable plexiform neurofibromas based on the KOMET trial.
Only about 2% of cases of rhabdomyosarcoma primarily arise from the chest wall, and such cases require careful planning.

Global ovarian and uterine cancer cases due to high BMI have risen sharply over the past 30 years, especially in low- to middle-income sociodemoraphic regions.

Speakers at AMCP Nexus 2025 reviewed the oncology pipeline, highlighting expanded indications and new therapies advancing innovation, access, and value.

Nicoletta Colombo, MD, PhD, of the University of Milan-Bicocca, discussed the rationale behind paclitaxel with bevacizumab and pembrolizumab in ovarian cancer.

New reporting suggests obesity and diffuse large B-cell lymphoma (DLBCL) have shared genetic risk factors.

Treatment options for patients with small cell lung cancer (SCLC) who survive to a third line of therapy are insufficient, authors of a new study argue.
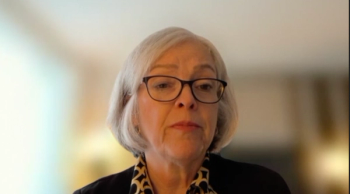
Susan Escudier, MD, FACP, of Texas Oncology, suggests actionable insights to improve equitable access to patient cancer care

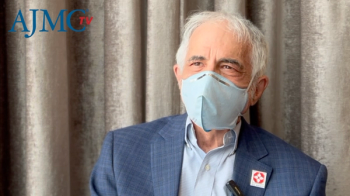
Payer contracts should incentivize the delivery of comprehensive, total-person cancer care, says Brian Mulherin, MD.
Many cancer survivors face ongoing physical and mental health challenges, which peer support and online resources can help address, says Brian Koffman, MDCM, DCFP, FCFP, DABFP, MSEd.

Despite systemic challenges, oncology practices use value-based care, community partnerships, and clinical trials to improve patient access and outcomes, says Brian Mulherin, MD.