Practical Implications of the FIDELITY Pooled Analysis
Rajiv Agarwal, MD, MS, considers the practical implications of the FIDELITY pooled analysis and how it may impact clinical practice.
Episodes in this series

Transcript:
Rajiv Agarwal, MD, MS: The most important recognition from this analysis is that if you’re a primary care doctor, a cardiologist, an endocrinologist, or a nephrologist, you can no longer rely on eGFR [estimated glomerular filtration rate] to detect kidney disease. That was yesterday, and that was 10 years ago. In 2021, you have to be looking at urine. If you have an ACR [albumin-to-creatinine ratio] of more than 30 mg/g, you need to be on finerenone if you have type 2 diabetes. Why? Because you’ve got CKD [chronic kidney disease]. If a patient’s potassium is 5 mmol/L or less, you can support them on finerenone and appreciate these risks.
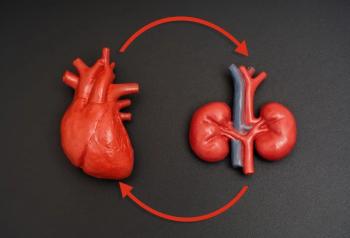
The big benefits in this population include hospitalization for heart failure. Even when we look at the pooled analysis, there’s a 22% relative risk reduction for heart failure hospitalization in the pooled analysis, and the P value is .003. Cardiovascular [CV] death is reduced about 12%, which isn’t significant because the upper bound of the hazard ratio is 1.02. But the composite outcome, the CV outcome, is 14%. It’s largely driven by heart failure hospitalization, somewhat by CV death, and nonfatal MI [myocardial infarction] reduced by 9%. Stroke isn’t really impacted. What we’re learning is that if you want to protect the heart, you can simply look at the urine and get an idea that this patient is at high cardiovascular risk. You don’t need any ejection fraction, HFrEF [heart failure with reduced ejection fraction], or HFpEF [heart failure with preserved ejection fraction]. All you need is the fraction of the urine albumin. That’s it: albumin-to-creatinine ratio. If that’s elevated, then you’re a candidate for finerenone.
That’s how it can change your practice. You don’t need to order an echocardiogram. You’d simply need to look at the urine albumin-to-creatinine ratio. Any patient who comes to your office can pee in a cup, and you send it to the lab and get a result. If it comes back elevated and the patient has type 2 diabetes, then they’re eligible for finerenone. It’s not academic anymore, because you’re making a dent in the heart and kidney failure outcome. When we look at the kidney failure outcome, the data are even more incredible. When we look at any component of the kidney failure outcome, short of renal death, we saw only 6 patients in the 2 trials—6 patients of 13,000—who died from kidney failure.
We can’t compute a confidence interval for the hazard ratio that’s of clinical value. However, when we look at end-stage kidney disease—that means going on dialysis or transplantation—it’s reduced 20%. eGFR less than 15 mL/min is reduced 19%. The 57% eGFR decline is reduced 30%. No matter how you look at it, the data look very promising for kidney failure, especially if you can tell your patient that if they take this drug, then they have a 20% less chance of going on dialysis than if they don’t take the drug. That’s very meaningful information that you can provide for the patient.
Transcript edited for clarity.
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.