Results From the EMPEROR-Pooled Analysis
Rajiv Agarwal, MD, MS, reflects on pooled data from the EMPEROR-Reduced and EMPEROR-Preserved trials.
Episodes in this series

Transcript:
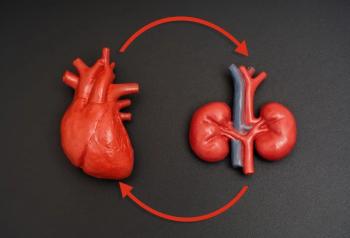
Rajiv Agarwal, MD, MS: The results presented were published in the New England Journal of Medicine by Dr Milton Packer and colleagues. They compared the results of kidney failure outcomes in the EMPEROR-Reduced and EMPEROR-Preserved trials. In the EMPEROR-Reduced trial, kidney failure outcome favors empagliflozin. This is the 40% kidney failure composite. But when you look at the EMPEROR-Preserved trial, there’s no difference in that regard between the 2 drugs. When you look at the surface to see what’s happening, it turns out that a number of things might be happening. One, when you take patients with HFrEF [heart failure with reduced ejection fraction], it might improve their cardiac output. It might improve the kidney perfusion. It might do many things that might not happen in the HFpEF [heart failure with preserved ejection fraction] population; therefore, you’re seeing a kidney-specific benefit. In fact, when you look at the slopes, there’s a greater preservation of the slope in HFrEF compared with HFpEF.
There’s a statistical benefit in the slope preservation in both trials, but it’s greater in patients with HFrEF. It tells you that the heart and kidney are strongly interlinked. If we improve heart function in HFrEF by improving ejection fraction, it might preserve the slopes but also protect from kidney failure, as we saw in the HFrEF trial. In the HFpEF trial, although there’s a preservation of the slope, there’s no signal for harm in terms of the kidney failure outcomes that look at 40% eGFR [estimated glomerular filtration rate] decline, etc. I don’t think the results are internally inconsistent. There are probably differences in the level of albuminuria in the 2 populations, and other characteristics that are hard to control for across trials that might contribute to these differences in these seemingly disparate outcomes. But I don’t think this is of great surprise. To the patient, it means you can use these drugs. They’ll keep you out of the hospital, breathing better, and they’re not dangerous to the kidney. If you have HFrEF, it might even protect your kidney. But if you have HFpEF, it’s not harmful for your kidneys.
For the cardiologists and primary care physicians who treat these patients, these are incredibly useful drugs. The challenge is going to be how we get the prescriptions written for these drugs because, as you saw in the FIDELITY analysis, barely 7% of patients who might be otherwise eligible for the drugs are on SGLT2 inhibitors. What I often see is that everybody passes the buck to the endocrinologist, and they say, “It’s a diabetes drug. It’s not my drug. The endocrinologist ought to write it.” Or the cardiologist might say, “It’s not my drug. The endocrinologist will write it.” I’ve seen nephrologists and primary care physicians say the same thing. These are drugs that might have an adverse effect of glucose-lowering, but they have an important benefit on the kidney and the heart as much like the ACE inhibitors and ARBs.
They had an adverse effect of blood pressure lowering, but they really protect the kidney and heart. Just as ACE inhibitors and ARBs have become the mainstream therapies for all physicians out there, SGLT2 inhibitors ought to be embraced by anybody who’s treating patients with type 2 diabetes and albuminuria and kidney disease, including HFpEF and HFrEF, particularly the cardiologists. They need to learn about it because they need to start prescribing these drugs. That’s the only way forward.
Transcript edited for clarity.
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.