Results From EMPEROR-Preserved: CV Outcomes in Patients With HFpEF
An overview of and results from the EMPEROR-Preserved trial, which tested the effects of empagliflozin in patients with HFpEF.
Episodes in this series

Transcript:
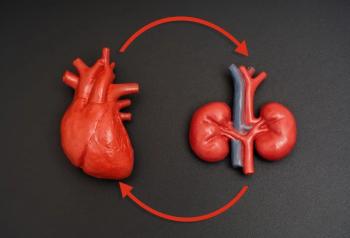
Rajiv Agarwal, MD, MS: The EMPEROR-Preserved trial was done in patients with heart failure with preserved ejection fraction [HFpEF], and they were randomized to a fixed dose of empagliflozin 10 mg vs placebo on top of standard of care. The results were nothing short of spectacular. They saw an improvement in the composite outcome of hospitalization for heart failure, MI [myocardial infarction], stroke, or cardiovascular death. These results are practice changing, especially in the context of patients with heart failure with preserved ejection fraction. This population hasn’t had any therapies previously approved.
Most of the available therapies are for HFrEF, or heart failure with reduced ejection fraction. This is the first time we’re showing an incredible benefit. We also showed, in this trial, that you have improvement in the slopes of decline of GFR [glomerular filtration rate], but there’s not any difference in the placebo group or the treatment group in the kidney failure composite outcome, which is 40% decline in eGFR [estimated glomerular filtration rate], ESRD [end-stage renal disease], or death from kidney failure. All in all, the study tells us that this might be a valuable drug for patients with heart failure with preserved ejection fraction, for which there are no approved therapies out there.
There’s an interesting result in the EMPEROR-Preserved trial in that the slopes of the GFR are different between placebo and empagliflozin. In fact, empagliflozin seems to be preserving the slope of eGFR decline. Yet when you look at the outcome of 40% decline in eGFR, kidney failure, or renal death, it’s no different. People might think that these are disparate results: how can you have protection of eGFR but no difference in outcomes? Well, there might also be different constructs that we’re looking at. In people who have 40% decline in eGFR events and end-stage kidney failure events, these are more distal events. The eGFR slope events can be analyzed in anyone who has a measurement of serum creatinine at a given time point. You can calculate the slopes easily, whereas with kidney failure outcome, it takes time to evolve.
Second, whenever you’re using a drug that has hemodynamic effects, you’re disadvantaging the drug that has the hemodynamic effect in reaching an earlier time point, such as a 40% eGFR decline. What do I mean by that? You’re looking at the time to first event, so if somebody has a 40% eGFR decline event, you take that person out of the pool. They don’t contribute to the second event of end-stage kidney disease for this end point. If you’re looking at empagliflozin, it basically reduces your eGFR acutely; therefore, you’re closer to the 40% eGFR decline end point compared with placebo. You might not see a difference in that end point. However, if you raise the bar to 57%, you might see a difference. If you raise the bar even higher to end-stage kidney disease, you might see a difference. But this isn’t a trial being done in patients with large amount of propionic acidemia, which is the primary driver of end-stage kidney disease in people with type 2 diabetes and CKD [chronic kidney disease].
We have to be careful in looking at these end points in isolation because you might say it’s not protecting the kidney in this population. Well, it is in terms of slopes, but it’s not showing you harm in terms of end-stage kidney disease. I’d say that the 40% eGFR decline end point and end-stage kidney disease is more about the harm that you’re measuring with empagliflozin and HFpEF, and you have no signal for harms. There may be some benefit, in the sense that the slopes are different between the 2 drugs. They’re probably 2 different constructs, and it’s of little surprise to nephrologists when they look at these data.
Transcript edited for clarity.
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.