- August 2020
- Volume 26
- Issue 7
Where Myths Go to Die
From the Editor-in-Chief, Evidence-Based Oncology, August 2020.
Yes
You have come upon the fabled lands where myths
Go when they die.
— James Fenton
The Pitt-Rivers Museum (1983)
As a medical student, I was struck by the number of times our teachers regaled us with the “Gordian Knot” myth as a paradigm for how we should approach understanding complex patients and seemingly indecipherable clinical data sets. As legend has it, the Gordian Knot was so complex that it was impossible to perceive where one strand began and another ended; thus, it could never be unraveled. The task was considered so great that anyone who could untie the knot was prophesized to become the ruler of a vast portion of the world as it was then known. According to one version of the legend, Alexander the Great considered the knot, and in a stroke of genius pulled out his sword and sliced the knot in half. In doing so he fulfilled the oracle’s prophesy. The lesson of this story, as espoused by my teachers, was that a simple solution frequently existed for most complex healthcare conundrums.
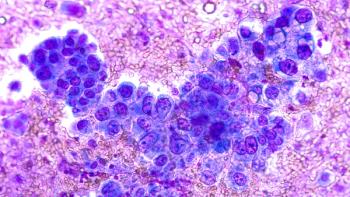
We now find ourselves in the midst of a golden era of cancer care in which insights gleaned from genomic data and our ability to leverage a growing armamentarium of targeted anti-cancer treatments routinely produce superior survival outcomes with an improved quality of life for many patients. Yet, these advances have come with questions and challenges about how to pay for these treatments, how to deliver them equitably to patients in need, and how to ensure that our systems of care become more patient-centered. Clinical reimbursement systems now repeatedly lag advances in cancer diagnostic and treatment technologies. The cost of some treatments (such as CAR T-cell therapies) have challenged existing payment models from both public and private payers. At the same time, our care portfolio continues to outpace our systems for delivering this care in financially sustainable ways. Rather than empower a path toward sustainable solutions, the naïve believe that a simple approach is possible. This has paralyzed us from coming to terms with the necessary complexity of what it will take to deliver precision medicine solutions to cancer patients in the future. It is time for the mythic “Gordian Knot” approach to the development of more effective and efficient cancer care delivery systems to die.
In this edition of Evidence-Based Oncology™ we look at the emergence of additional innovative anti-cancer treatments, such as the second generation of the BTK inhibitors, DNA-based therapies for glioblastoma patients, and the clinical opportunities for the detection of NRG1 gene fusion in selected patients. Beyond exploring new diagnostic and therapeutic opportunities for cancer patients, we also review the exciting potential avenues for how healthcare payment and clinical reimbursement might evolve to support sustainable delivery of innovative treatments. Mark Trusheim, MSc, of MIT discusses a long-awaited plan to improve the ability of Medicaid programs to pay for gene-based therapeutics. Keely Macmillan, MSPH, from Archway Health discusses how downside risk related to precision oncology and high-cost therapeutics can be sustainably managed in the context of oncology advanced alternative payment models.
As the practice and systems-based delivery of cancer care evolves at a breakneck pace, simple solutions are more likely to harm, than help, essential stakeholders. Effective new delivery and payment systems can only emerge, however, if healthcare leaders fully embrace the inescapable necessary complexity of creating these systems. The writer HL Mencken cynically noted that, “For every complex problem there is an answer that is clear, simple and wrong.” There are many avenues in which the “Gordian Knot” approach leads to false choices and ill-conceived simple solutions. Pithy myths are a poor paradigm for navigating complex dilemmas. The path toward the broad realization of innovative, financially sustainable, equitably-delivered cancer care is likely to be an arduous, painful journey. It is time to embrace that complexity and let the comforting myths die.
https://doi.org/10.37765/ajmc.2020.88485
Articles in this issue
over 5 years ago
FDA Actions Include Third CAR T-cell Therapyover 5 years ago
Best Cancer Tests Don't Reach All Who Need Themover 5 years ago
Choice Is Vital to Biosimilar Savings Picture, Panelists Sayover 5 years ago
MRD, Biomarkers in Multiple Myelomaover 5 years ago
Hospitals Vow to Fight Court of Appeals 340B RulingNewsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.