In a recent study, researchers detailed the use of various biosensors for minimal residual disease (MRD) detection in non–small cell lung cancer (NSCLC).
Jaime is a freelance writer for The American Journal of Managed Care® (AJMC®), where she previously worked as an assistant editor.
She has a BA in print journalism from Penn State University. You can connect with Jaime on LinkedIn.
In a recent study, researchers detailed the use of various biosensors for minimal residual disease (MRD) detection in non–small cell lung cancer (NSCLC).

The recommendations come at a time when treatments for chronic lymphocytic leukemia (CLL), such as venetoclax, are making deep remissions and undetectable minimal residual disease (MRD) after a fixed duration of treatment feasible goals.
The data set included 177 samples from polycythemia vera, essential thrombocytopenia, primary myelofibrosis, and healthy donors, from which the researchers found that MAPK14 was overexpressed in PV samples and was associated with more symptoms and worse outcomes.

The approach works by transforming the condition of normal and tumor cells into a highly proliferative “reprogrammed stem-like” condition that still has the original karyotypes.

The findings showed that between 2009 to 2016, 76% of the 122 patients included in the study were on sick leave a year following their allogeneic hematopoietic stem cell transplantation (allo-HSCT).

The drug sensitivity test-guided treatment was associated with significant improvements in the patient’s condition after 8 weeks.
According to the study authors, a growing number of findings from preclinical studies have suggested a focus on immunometabolism to modulate alloreactive donor T cell responses to control graft-versus-host disease (GVHD) and promote graft-versus-tumor effect.

To date, just 3 previous reports have detailed cases of mitochondrial malate dehydrogenase deficiency (MDH2D), and there are no known cures.

Across all studies included, observed-to-expected ratios showed that White and Asian patients were overrepresented while Black patients, Hispanic patients, and American Indian/Alaskan Native patients were underrepresented.

These second-generation inhibitors include acalabrutinib, zanubrutinib, and tirabrutinib, and researchers hope they can overcome the off-target toxicity and treatment resistance that can be experienced with ibrutinib.

Findings from this new study are the result of an investigation into over 360 children, many with active hepatitis, elevated alanine aminotransferase levels, and an immune active phenotype.

Immune-mediated necrotizing myopathy typically presents with progressive symmetrical proximal muscle weakness and myalgias, although some cases can present with respiratory and esophageal muscle weakness, as seen in this reported case study.

Researchers argue that Onodera’s prognostic nutritional index, calculated by lymphocytes and serum albumin to determine nutritional and immune status, is a straightforward method for use among patients undergoing liver surgery.
In a recent paper, researchers outlined the utility of minimal residual disease (MRD) among patient with acute lymphoblastic leukemia (ALL) and how its monitoring at specific timepoints has proven useful for stratifying patients and helping to ensure appropriate treatment decisionsMRD

The current study found that those prescribed potentially inappropriate medications were actually less likely to revisit the emergency department within 30 days, in contrast to prior work.

The study of 36 patients showed a response rate of 59% at 3 months, which increased to 62% at 6 months.

Unlike the success seen in other cancer types, biomarker-driven treatment advances in gastroesophageal adenocarcinoma (GEA) have been hindered by its genomic heterogeneity. A significant proportion of patients also develop resistant subclones through selective pressure, resulting in disease progression.

The data offer novel insights, as comparable data on the drug class is scarce despite 2 JAK inhibitors being approved for use in myelofibrosis and others showing promise.

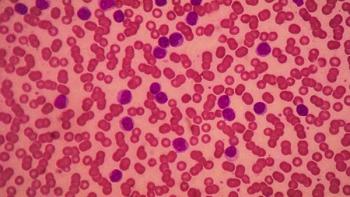
Complications of note in patients with myeloproliferative neoplasm (MPNs) include ischemic stroke, intracerebral and subarachnoid hemorrhage, microbleeds, posterior reversible encephalopathy syndrome, and dural sinus and cerebral vein thrombosis.

From the decision analysis came an agreement that reimbursement for an orphan drug should be based primarily on its effect on health-related quality of life, its effectiveness, and the availability of other treatment options.

According to researchers, new findings may have important implications for expanding the use of measurable residual disease (MRD) in multiple myeloma.

In a recent study, researchers were able to show how different evolutionary forces in aging blood stem cells impact whether or not someone develops acute myeloid leukemia (AML), offering insight into those at higher risk of the disease.

Unlike most other cancers, the progression of hairy cell leukemia is largely driven by extended cell survival rather than increased proliferative cell fractions.
Ruxolitinib is increasingly being used in patients with graft-vs-host-disease (GVHD); a recent study found a link with transplant-associated thrombotic microangiopathy (TA-TMA) in patients with GVHD treated with the therapy.
The murine study, which assessed the combination of foretinib and an anti–PD-1 antibody, found that the regimen enhanced antitumor activity, offering promise in a cancer that has seen less success with immunotherapies than others.
Most studies to date that show efficacy with ruxolitinib in this setting have been in adult patients.

The study, using a BCR/ABL1 assay, found that the novel method is able to detect minimal residual disease (MRD) in a larger range of patients compared with quantitative real‐time polymerase chain reaction, the method currently used to detect MRD.
The findings, if confirmed in subsequent research, could prove to have significant implications, as only a small subset of patients with chronic lymphocytic leukemia (CLL) respond to chimeric antigen receptor (CAR) T-cell therapy.

This study protocol comes amid a paradigm shift in the treatment of advanced-stagen non–small cell lung cancer (NSCLC) following the emergence and uptake of immunotherapy.

The meta-analysis collected findings from 11 studies, from which researchers determined statistical heterogeneity regarding the incidence of GVHD between patients receiving only HSC transplantation or only killer cell therapy, and patients receiving HSC transplantation in addition to killer cell therapy.

259 Prospect Plains Rd, Bldg H
Cranbury, NJ 08512
© 2025 MJH Life Sciences®
All rights reserved.
