Atopic Dermatitis
Latest News

Latest Videos

CME Content
More News

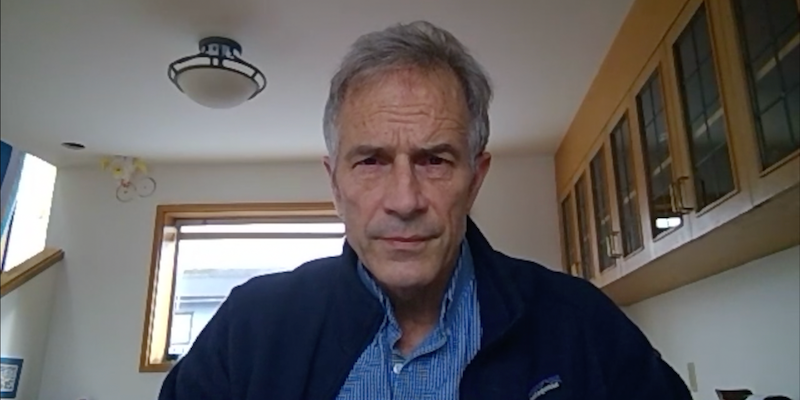
Robert Sidbury, MD, MPH, chief of the Division of Dermatology at Seattle Children's Hospital, discusses risk factors involved in the pathogenesis of atopic dermatitis and several diagnostic methods.

Japanese children of parents whose family business was primarily industry, including agriculture, forestry, and fisheries, had a greater risk of atopic dermatitis (AD) development.

Children with moderate to severe atopic dermatitis were found to be more likely to report suboptimal sleep and attention regulation outcomes.

Robert Sidbury, MD, MPH, chief, Division of Dermatology, Seattle Children's Hospital, speaks on the inflammatory mechanisms of atopic dermatitis and risk of comorbidities in affected patients.

The JAK1 inhibitor abrocitinib (Cibinqo) was recently approved by the FDA for the treatment of adults with refractory, moderate to severe atopic dermatitis.

Minority patients and those with low income were more likely than White and high-income counterparts to report adverse outcomes in the management of asthma and eczema.

Researchers review current knowledge on the management of flares in atopic dermatitis, including treatment and unmet needs.

Patients with atopic dermatitis (AD) treated with dupilumab showed reduced hospitalization rates and shorter duration of AD-related hospitalizations vs those treated with control therapies.

Patients with atopic dermatitis were associated with significant economic burden primarily driven by outpatient visits and pharmacy use, which increased with disease severity.

Incidence of infectious diseases, skin infections, and systemic antibiotic exposure were all associated with the development of atopic dermatitis among infants and young children.

Patients with atopic dermatitis were shown to be more likely to receive a COVID-19 diagnosis than the general population.

Children and adolescents with atopic dermatitis (AD) tended to have a higher number of delinquent behaviors than those without AD, including fighting, cheating on exams, and suspension.

Korean patients with moderate-to-severe atopic dermatitis achieved and maintained markedly improved skin clearance with dupilumab treatment in a real-world setting, including in the face and hands.

David R. Stukus, MD, FACAAI, of Nationwide Children's Hospital and The Ohio State University College of Medicine, and a board member of the American College of Allergy, Asthma & Immunology, speaks on the lack of interventions to manage the underlying causes of exacerbation in atopic dermatitis.

A study found significant differences in the therapeutic and diagnostic approaches to atopic dermatitis used by allergists, dermatologists, and pediatricians, and those recommended by guidelines.

David R. Stukus, MD, FACAAI, of Nationwide Children's Hospital and The Ohio State University College of Medicine, and a board member of the American College of Allergy, Asthma & Immunology, speaks on the difficulties of gaining coverage for newer biologic therapies in the treatment of atopic dermatitis.

Research presented at the Revolutionizing Atopic Dermatitis (RAD) Virtual Conference said dupilumab (Dupixent) is an effective and safe therapeutic option in adults, adolescents aged 6 to 11 years, and young children aged 6 months to 5 years with moderate-to-severe atopic dermatitis.

David R. Stukus, MD, FACAAI, of Nationwide Children's Hospital and The Ohio State University College of Medicine, and a board member of the American College of Allergy, Asthma & Immunology, discusses efforts to align novel treatments for atopic dermatitis with patients based on the underlying mechanisms of disease.

In a new review article, investigators outline the challenges to studying the disease, but also point to big data as an important tool moving forward.

Patients with atopic dermatitis, particularly those with more severe skin manifestations, were shown to be at greater risk of depression and anxiety compared with the general population.

Children with atopic dermatitis were shown to be at an increased risk of fractures compared with the general population, with systemic use of corticosteroid and antihistamine therapy cited as mediating factors.

A high comorbidity burden, including psychiatric, autoimmune, and systemic conditions, was found in US adult ambulatory populations with atopic dermatitis.

More than 1 in 3 patients with atopic dermatitis reported incidence of dupilumab-induced ocular surface disease (DIOSD), with asthma and family history of AD shown to further increase the risk of developing DIOSD.

Moderate-to-severe disease, childhood onset, and systemic treatments were all associated with a greater risk of conjunctivitis in patients with atopic dermatitis, whereas use of soft and hard contact lenses were linked with risk of keratitis.

Findings of a machine learning-based deep phenotyping approach found a myriad of factors associated with severe disease in atopic dermatitis, including age between 12 and 21 years or older than 52 years, lack of physical activity, and incidence of alopecia areata.