
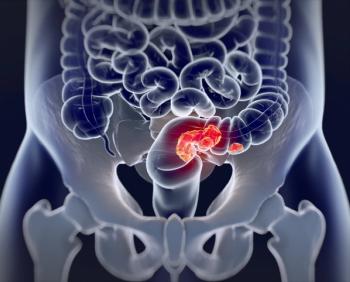
Lowering the positivity threshold for a high-quality fecal immunochemical test (FIT) can increase sensitivity of noninvasive screening for colorectal cancer in a more economical way.

Lowering the positivity threshold for a high-quality fecal immunochemical test (FIT) can increase sensitivity of noninvasive screening for colorectal cancer in a more economical way.

Risk factors of colorectal cancer (CRC) include both smoking and a combination of smoking and alcohol in African patients.

Low- and high-income countries had significant disparities in screening for colorectal cancer (CRC) due to limited access to screening and treatment in low-income countries.

Ratios of visceral proteins can act as independent indicators for both overall and progression-free survival in patients with colon cancer.

As rates of CRC skyrocket in young individuals, means of addressing the growing problem must be considered.

Results could vary between having a net benefit or harm based on the balance between achieving screening in individuals who otherwise wouldn’t and using cell-free DNA blood tests in favor of more effective methods of screening for colorectal cancer (CRC).

Surgery for colorectal cancer has been both positive and challenging when using robotic-assisted surgeries.

Patients were found to have similar completion and yield rates for the fecal immunochemical test (FIT) at both 45 years and 50 years, making screening for colorectal cancer (CRC) effective in younger patients.

While treatment options are evolving cancer care and extending lifespans, there is still a lack of biomarkers in certain cancers that can help direct treatment or provide early detection.

Patients with refractory metastatic colorectal cancer could use trifluridine/tipiracil (TAS-102) plus bevacizumab as a cost effective third line treatment in China but the same was not found in the United States and United Kingdom.

The updated guidelines from the US Preventive Services Task Force (USPSTF) have led to an increase in screening for colorectal cancer (CRC) in individuals aged 45 to 49 years.

Increased time spent on discussing testing for colorectal cancer (CRC) was associated with patient satisfaction in older adults.

Patients with colorectal cancer (CRC) liver metastases had reduced risk of intrahepatic recurrence when using intraoperative contrast-enhanced ultrasounds.

Colorectal cancer (CRC) could be affected by various factors involved in sleep, including snoring.

A substantial overall survival (OS) disparity by race and ethnicity was found in patients with colorectal cancer (CRC), with socioeconomic status and tumor molecular features largely contributing to the difference in OS.

An update to the colonoscopy guidelines released by the American College of Gastroenterology and the American Society for Gastrointestinal Endoscopy could have implications on how colonoscopies are measured in the future.
Patients who received radiotherapy without a recurrence of rectal cancer had significantly lower quality of life compared with patients who did not receive radiotherapy.

Educational principles implemented after 1998 may have led to lower mortality rates in patients with colorectal cancer (CRC) receiving care from doctors trained after that point.

Early-stage detection of colorectal cancer (CRC) could be achieved using a noninvasive multiomics liquid biopsy test, according to a recent study.

The new guidelines are another method of keeping a high-quality standard for colorectal cancer screening.

Cancer detection was slower to rebound after the COVID-19 pandemic compared with endoscopic activity, specifically in gastric cancers such as colorectal cancer.

Many patients could be at risk of colorectal cancer (CRC) without realizing as most patients don’t know if their immediate family has had CRC.

Although the FDA approval of Guardant Health’s Shield blood test provides an appealing alternative to other colorectal cancer screening methods, the advantages and disadvantages should be highlighted with patients.

Patients with symptoms of gastrointestinal (GI) problems and survivors of colon cancer were more likely to use oncology specialty care.

A simple, user-friendly decision-making model that used self-reported information was able to perform well in outpatient decision-making for patients with colorectal cancer (CRC).

259 Prospect Plains Rd, Bldg H
Cranbury, NJ 08512
© 2025 MJH Life Sciences®
All rights reserved.
