Center on Health Equity & Access
Latest News
Latest Videos

CME Content
More News

The machine learning model shows promise in detecting paroxysmal nocturnal hemoglobinuria (PNH) by assessing electronic health records (EHR) data, potentially transforming the diagnostic landscape for rare diseases.

The policy community should consider these concrete suggestions to address the challenges presented by social determinants of health.

A recent retrospective, cross-sectional study found that detecting self-injurious thoughts and behaviors in youth requires improvement to ensure equitable identification of at-risk patients.

Prompt care supports mental well-being, as hidradenitis suppurativa is often associated with depression and anxiety due to its physical and social challenges.

The Center on Health Equity & Access focuses on addressing disparities in health care access, exploring innovative solutions, policies, and research to improve health equity across diverse populations.

The Dobbs decision was associated with a 7% absolute increase in overall infant mortality—equivalent to 247 excess deaths—and a 10% increase among infants with congenital anomalies, corresponding to 204 additional deaths.
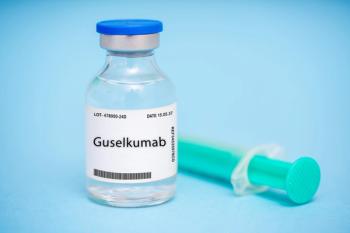
New phase 3b data reveal significant skin clearance in historically underserved patients with moderate plaque psoriasis, offering hope for improved treatment outcomes.

The Medicaid budget survey for fiscal years 2024 and 2025 revealed state predictions are expecting a decline in Medicaid enrollment and an increase in spending next year due to the end of pandemic-era policies and federal funding.

Of the 10% of women contacted for this survey who said that they or their partner had ever sought fertility assistance, only 7% were able to get the necessary care; cost was cited as the top reason for not being able to access fertility services.

There can be a delay in diagnosis of myeloproliferative neoplasms as the symptoms of the diseases can be variable and common, such as fatigue, migraines, and difficulty concentrating, explained Ruben Mesa, MD, of Atrium Health.

On this episode of Managed Care Cast, we're talking with the author of a study published in the October 2024 issue of The American Journal of Managed Care® that explored prior authorization decisions in cancer care by race and ethnicity for commercially insured patients.

Medicaid, Medicare, and private insurance programs all showed significant variability in expenditures based on social and nonclinical factors.

Among near-poor Black and Hispanic individuals, Medicare Advantage was associated with increased vision care and some, although not uniform, reductions in access disparities vs traditional Medicare.

Groundbreaking proposal to expand contraception coverage under the ACA marks the most significant update in over 10 years.

In our conversation with Jeff Giullian, MD, MBA, chief medical officer with DaVita Kidney Care, we dive into 4 important aspects of kidney care: prevention, social support, integrated care, and patient support.

Many women remain unaware that the Affordable Care Act (ACA) mandates cost-free preventive services; however, ongoing legal challenges threaten the future of this coverage.

The Center on Health Equity & Access focuses on addressing disparities in health care access, exploring innovative solutions, policies, and research to improve health equity across diverse populations.

The history of women being left out of heart disease research has had significant consequences on heart health care today.

Hidradenitis suppurativa (HS) is an inflammatory, chronic disease with very high symptom and physical burdens, and it can get progressively worse over time if it's inadequately treated, explained Amit Garg, MD, founding chair, Department of Dermatology, Northwell Health.

The current research focus for Umit Tapan, MD, Boston Medical Center, is reducing disparities in lung cancer care and improving treatment access, in particular for immunotherapy and targeted treatments.
New findings show that undocumented Latinx immigrants, who make up 7% of the US population, face significant challenges in accessing health care due to uninsurance, limited access to care, language barriers, and fears surrounding their immigration status.

Early Intervention, Targeted Strategies Needed to Improve Disparities, Survival in Patients With IPF
Two posters presented at the CHEST 2024 annual meeting highlighted the importance of addressing socioeconomic disparities and identifying clinical predictors to improve outcomes and survival rates among patients with idiopathic pulmonary fibrosis (IPF).

Bipolar disorder is commonly misdiagnosed depending on the features that present, explained Stephanie Hsia, PharmD, MAEd, BCPP, of University of California, San Francisco.
Despite advancements in umbilical cord blood transplants, social determinants of health, such as poverty and public insurance, continue to impact outcomes, underscoring the need for equitable access to lifesaving treatments.

Two posters presented at the CHEST 2024 annual meeting highlighted significant disparities in acute coronary syndrome care and outcomes among different racial, ethnic, and gender groups, underscoring the urgent need for targeted interventions to address these inequities.