
Health Care Cost
Latest News
Latest Videos

CME Content
More News

The findings highlight the significant financial burden of sickle cell disease.

United States birth rate rises from last year but is still lower than pre-pandemic; a drug plant closure in California could affect availability of 5 essential medications; the No Surprises Act prevented 2 million potential surprise bills in first 2 months of 2022, report says.

Dupilumab was associated with reductions in exacerbations and oral corticosteroids (OCS) dosage, as well as improved lung function, in patients with OCS-dependent asthma with and without comorbid chronic rhinosinusitis with nasal polyps.

Chargemaster lists may encourage patients to shop around for services, but the authors of this report said the implications of this change for dermatology are not well-defined.

Across commercial insurance, Medicare, and Medicaid populations, oncology is the top category of spend, and the drug pipeline has increasing specific and complex therapies.

Today, health plans are shifting dollars to more value-based contracts along with investments in population health management. Digitizing lab results across all care settings and unlocking the potential of lab values can help health plans reach the Triple Aim of improving the patient experience, improving the health of populations, and reducing the per-member cost of health care.

The report details totals paid to hospitals by private insurers and providers and compares the sums with a Medicare benchmark.

Significantly greater persistence, adherence, and time on monotherapy was achieved with the use of ixekizumab vs the biologics adalimumab, etanercept, secukinumab, and ustekinumab, in the treatment of moderate to severe psoriasis.
Gene therapies in the pipeline to treat hemophilia will be very expensive, but they also seem to be very efficacious, and multiple could hit the market between now and 2024, said Ray Tancredi, RPh, MBA, CSP, divisional vice president, specialty pharmacy development and brand Rx/vaccine purchasing, Walgreens.

While CMS has started making changes to address health equity through policy and payment models, commercial plans are waiting to see the outcomes before they follow suit, said Jayson Slotnik, partner, Health Policy Strategies, Inc.

This study found extensive variation in general internal medicine physician prices and that high-priced physicians provided fewer low-value services but had higher spending on these services.

Biosimilar adoption can be accelerated or stymied depending on actions taken by the managed care space, explained Sonia Oskouei, PharmD, vice president, biosimilars, Cardinal Health, during a session at Asembia’s Specialty Pharmacy Summit.

The impact that the adalimumab biosimilars will have in 2023 is going to depend on when they all get to market, said Doug Long, MBA, vice president, industry relations, IQVIA.

US Senate to vote this week on legislation seeking to codify abortion rights into law; hospitals aiming to raise treatment prices in response to increasing nurse salaries; shortage of infant formula worsening nationwide.

UPMC Health Plan, RxAnte, and Mosaic Pharmacy Services outlined how they are operating a value-based pharmacy care management program within Community HealthChoices, Pennsylvania’s managed Medicaid long-term services and supports (LTSS) program, at a recent conference.

Future quality conversations must recognize what the pandemic has illustrated over the past 2 years—that patients who were in the most dire need of health care, including those with multiple chronic conditions, had the least amount of access, said Jonathan Blum, MPP, the principal deputy administrator and chief operating officer of CMS.

Coverage, equity, and value-based payments are critical areas of focus for the Biden administration’s health care agenda leading up to the midterm elections, according to 3 experts from Avalere.

Limited evidence from a literature review suggests that co-pay assistance was associated with improved treatment persistence/adherence across various diseases, with indirect evidence suggesting improvements in clinical outcomes.
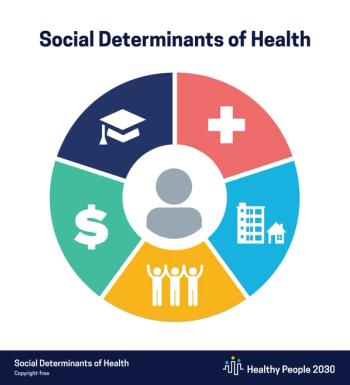
At the Pharmacy Quality Alliance (PQA) 2022 Annual Meeting Wednesday, participants heard about some unexpected insights arising from a workshop held this week between patients and pharmacists who are creating a patient-centered outcomes research agenda focused on addressing social determinants of health (SDOH) in the community pharmacy setting.

Atopic dermatitis was associated with the greatest burden of disease compared with 2 other types of dermatitis, in which high incidence and disability-adjusted life-years rates corresponded with high sociodemographic index areas.

Using socioeconomic status (SES) as their primary exposure, investigators from McGill University, University of Manitoba, Institut National de Santé Publique du Québec, and Laval University investigated reasons behind insulin pump uptake disparities in the Canadian provinces of Manitoba and Québec.

Adam Fein, PhD, of Drug Channels Institute, and Doug Long of IQVIA discussed trends in the specialty pharmacy market in the United States.

Representatives from employers, pharmacy benefit managers, and others discussed methods of improving pharmacy access and affordability in health plans.

Value-based payments were a benefit during the pandemic, but it remains to be seen if patients are interested in keeping those changes in care delivery as the pandemic recedes, said Jayson Slotnik, partner, Health Policy Strategies, Inc.

On this episode of Managed Care Cast, Ari D. Panzer, BS, lead author and researcher, then at Tufts Medical Center—now at Duke University—discusses the findings from his team’s investigation into coverage decisions by health plan insurers of the 66 drugs approved by the FDA in 2018.


















