Myelodysplastic Syndromes
Latest News
Latest Videos

CME Content
More News

The single-center report showed the therapy had a favorable safety profile and manageable side effects in children with relapsed or refractory (R/R) acute myeloid leukemia (AML) or myelodysplastic syndromes (MDS).

Rigorous surveillance of children at high risk for developing myelodysplastic syndrome (MDS) is especially warranted, according to researchers.

A new study finds that eliminating radiation from conditioning regimens in patients with dyskeratosis congenita undergoing allogeneic hematopoietic cell transplantation did not negatively affect survival or increase complications.
Physicians also differed from caregivers when asked how many hours of caregiving patients required each week.
A recent study evaluates the dosing, safety, and efficacy of telaglenastat and azacytidine to treat advanced myelodysplastic syndromes (MDS), with promising results.

The study is among the first to look at the potential impacts of clonal dynamics on patients with lower-risk myelodysplastic syndromes (MDS).

In recent years, it’s been estimated that 10% to 28% of patients with myeloid disorders develop adult onset inflammatory and autoimmune disorders (IADs), complicating treatment.

Results from a retrospective study compared and explored biomarkers associated with outcomes in myelodysplastic syndrome (MDS) with plasma cell neoplasms.

Celiac disease presents a higher risk for developing malignant neoplasms, including small intestine, lymphoma, and skin cancers, but presents a lower risk for respiratory malignancies.

New research linking telomere shortening to myelodysplastic syndromes (MDS) offers substantial therapeutic implications for affected patients and MDS research.

Patients with myelodysplastic syndromes report high satisfaction with oral decitabine/cedazuridine (DEC-C) vs traditional intravenous or subcutaneous hypomethylating agents.

The researchers found inferior outcomes and higher accrued costs associated with alloimmunization in patients with myelodysplastic syndromes (MDS), a disease that relies on transfusion of red blood cells.

Authors acknowledge that both the 2022 World Health Organization and International Consensus Classification myelodysplastic syndrome criteria sets have value, while sorting out their similarities and differences.

More and more hematology factors and parameters can be analyzed with advanced equipment to better pinpoint which patients might have myelodysplastic syndromes (MDS)—but the differences in leading makers’ systems can be tricky to maneuver.

Only about a quarter of patients who have myelodysplastic syndrome (MDS) experienced hematologic improvement with erythropoiesis-stimulating agents (ESAs).

Post–hematopoietic cell transplantation (HCT) prophylaxis using cyclophosphamide to stave off graft-vs-host disease had positive results compared with calcineurin inhibitor–based prophylaxis, regardless of whether the patient had a matched or unmatched donor.

The findings show most patients with low-risk myelodysplastic syndrome (MDS) will die before progression.

Patients with myelodysplastic syndrome (MDS) in the treatment arm were more likely to achieve transfusion independence, but the difference vs placebo was not statistically significant.
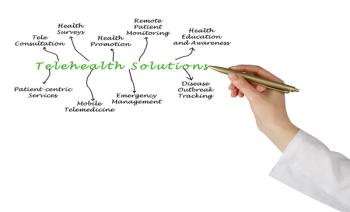
Researchers collected feedback from 20 clinicians implementing a telehealth serious illness conversation (SIC) with their patients with acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS).

In a recently published systematic review, researchers determined that VEXAS (vacuoles, E1 enzyme, X-linked, autoinflammatory, somatic) syndrome typically presents in men, with atypical morphology and with systemic symptoms.

Study findings provide new tools to assess treatment preferences when using hypomethylating agents in myelodysplastic syndromes (MDS).
Determining the roles that various inflammatory markers and pathways play in lower-risk myelodysplastic syndromes (MDS) could lead to therapies that keep disease progression at bay.

Researchers have identified a causal link between gut microbiota and myelodysplastic syndrome (MDS) risk, mediated by certain key immune cell phenotypes.

The coalition said, however, that patient-reported outcomes (PROs) in the myelodysplastic syndrome (MDS) space will be most meaningful if they are collected rigorously and if the data are transparent.

Hemoglobin levels, transfusion independence, and low serum erythropoietin levels were all deemed to have a statistically significant relationship with erythropoiesis-stimulating agent (ESA) response.