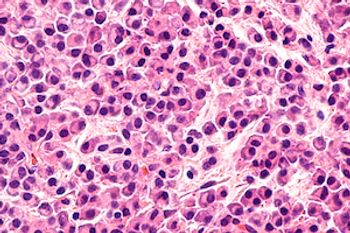
Currently, minimal residual disease testing is being used for prognostication not for treatment decisions, explained Thomas G. Martin, MD, clinical professor of medicine, Adult Leukemia and Bone Marrow Transplantation Program, associate director, Myeloma Program, University of California, San Francisco (UCSF); co-leader, Hematopoietic Malignancies Program, Helen Diller Family Comprehensive Cancer Center.