
Payers
Latest News
Latest Videos

Podcasts
More News

A new survey reveals widespread consumer frustration with prior authorization, highlighting the need for urgent reform in insurance coverage.

This article examines the prevalence of pay-for-performance incentives to promote human papillomavirus vaccination and other quality metrics as reported by frontline clinical staff.
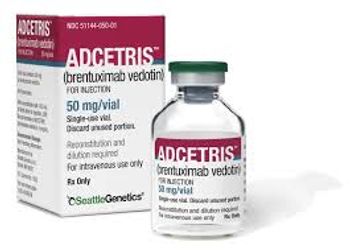
Brentuximab vedotin combined with cyclophosphamide, doxorubicin, and prednisone (CHP) shows promising results as a first-line treatment in newly diagnosed peripheral T-cell lymphoma (PTCL).

There is a great need to streamline the process from the tissue sample to the diagnostic lab, whether it's genomic or immunohistochemistry, Robert Kratzke, MD, says.
Revumenib is now the sole targeted therapy recommended by the National Comprehensive Cancer Network for KMT2A-rearranged acute leukemia, which opens a path for payers, said Ivo Abraham, PhD, RN, of The University of Arizona.

Sadie Dobrozsi, MD, of Evolent, discusses how predictive genomics is pushing cancer care into a new era of personalization

Jayme Ambrose, DNP, RN, CCM, of Adobe Population Health, explores how addressing social determinants of health transforms maternal care delivery, reduces disparities, and improves outcomes for mothers and infants.

Artificial intelligence (AI) transforms oncology by enhancing clinical decision-making, improving patient outcomes, and shaping future health care training, as discussed by experts at Tennessee Oncology's “Tech Innovations in Community Oncology."

Families caring for individuals with Duchenne muscular dystrophy (DMD) face significant financial burdens from necessary home and vehicle modifications to enhance quality of life.

During the “Tech Innovations in Community Oncology” meeting from Tennessee Oncology, oncologists explore artificial intelligence (AI) tools like DeepScribe to enhance documentation efficiency, reduce burnout, and improve patient engagement in clinical settings.

Precision oncology has entered a new phase, as data sets mature and a new wave of tools emerges to help clinicians manage cancer care over time.
Revumenib for relapsed/refractory acute leukemias with KMT2A translocation is cost-neutral for health plans, but traditional methods of analysis may not be accurate for rare diseases, said Ivo Abraham, PhD, RN, of The University of Arizona.

Several evidence-based health literacy resources may be beneficial in health plan settings to improve organizational health literacy, personal health literacy, and health equity.

Coverage from IVBM Princeton, held May 8, 2025.

Pharmacists are being asked to not only manage medications and side effects but also be fiscally responsible for the whole institution and its trickle-down effect on costs, said David Awad, PharmD, BCOP, of Robert Wood Johnson University Hospital.

The Choose Medicare Act would establish a Medicare Part E that would give employers and the general public the ability to opt into the program.

A private oncology shared savings plan reduced colon cancer treatment costs. Results varied by tumor, with none in breast cancer and mixed effects in lung cancer.

Patients who remained on treatment, especially at higher doses or on tirzepatide, were more likely to achieve clinically meaningful weight loss and improved glycemic control.

Julia Lucaci, PharmD, MS, of Becton, Dickinson and Company, discusses the benefits of blister packaging for chronic medications, advocating for payer incentives to boost medication adherence and improve health outcomes.

Results for IRAKLIA show noninferiority for Sanofi's on-body delivery system for isatuximab, compared with IV administration. Patients overwhelmingly preferred the hands-free delivery option.
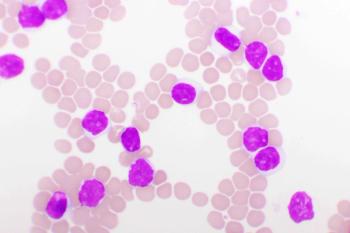
Zanubrutinib showed long-term efficacy in patients with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL) and deletion of the 17p chromosome, with progression-free survival similar to patients without high-risk disease characteristics.

Medicare Part B drug negotiations in 2028 pose challenges for providers, requiring new payment systems and strategies to ensure patient access, explained H. John Beardsley, MBA, of CoverMyMeds, and Fauzea Hussain, MPH, of McKesson.

A score was developed to measure patient risk from payer utilization management policies and its relationship to real-world US commercial payer utilization management policies.

Payers should consider providing higher reimbursement rates and/or preferred pharmacy networking status for pharmacies that provide chronic medications in blister packs for patients.





















