Insurance
Latest News
Latest Videos

More News
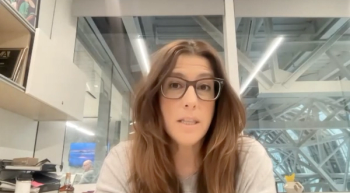
Carrie Kozlowski, OT, MBA, chief operating officer and cofounder of Upfront Healthcare, explains how the company emphasizes personalized engagement to overcome technological, cultural, and social barriers while Medicaid disenrollment rates are increasing.
Part of the recent Medicare reimbursement cuts could be addressed in a spending package next month; Medicaid/Medicare dual eligibles are expected to generate big profits for health insurers; FDA sent warning letters to online vendors selling unapproved and misbranded versions of semaglutide and tirzepatide.
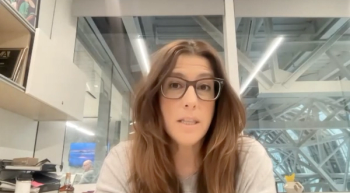
"I'll say what I don't think the issue is—it's not technology. We can solve this problem with technology," Carrie Kozlowski, OT, MBA, explains in the interview.

On this episode of Managed Care Cast, we're talking with the authors of a study published in the February 2024 issue of The American Journal of Managed Care® about their findings on how health plans can screen for health literacy, social determinants of health, and perceived health care discrimination.

The federal State Health Insurance Assistance Program (SHIP) provides counseling and education on Medicare coverage options. This article highlights potential inequities in in-person SHIP service access.
Over the past 20 years, Medicare physician pay has plummeted by 26% when adjusted for inflation, while hospital reimbursement has surged by 70%, prompting over 100,000 doctors to abandon independent practice for hospital or corporate employment since 2019.
Overcoming insurance hurdles for critical medications; rising heat and wildfires reverse decades of clean air progress; conflicts between parents and schools arise as teens seek mental health support

This study leverages newly available hospital pricing data to explore hospital-insurer contracts from a large hospital chain.

Catch up on this week's news at the Center on Health Equity and Access.

At an Institute for Value-Based Medicine® event held in Phoenix, Arizona, experts from Banner Health and Aetna discussed how health inequities and social determinants of health can affect primary care in patients with any type of insurance.

A provision in the Inflation Reduction Act will implement a $2000 out-of-pocket cap on Medicare beneficiaries’ prescription drug spending, which could save money for more than 1 million enrollees when it takes effect next year.
House Republicans voted to ban quality-adjusted life years (QALYs) from being used as a drug pricing metric in federal health programs; insurance executives disapproved of newly proposed 2025 Medicare Advantage (MA) rates; patients with long COVID enrolled in an online exercise program said their health improved more than people who received standard care.

Medicare coverage did not necessarily lead to increased diagnosis of chronic conditions.
A total of 16,430,000 Medicaid enrollees have been disenrolled across all 50 states and the District of Columbia, as of February 1, 2024.

Screening for Health Literacy, Social Determinants, and Discrimination in Health Plans
This study provides insight on the experiences of patients of a national health plan with 2 structural determinants of health—health care discrimination and health literacy—and how those interact with social determinants of health and patient demographics.

The article emphasizes the significance of accreditations in addressing health disparities and promoting health equity, highlighting programs for achieving accreditation and advocating for the integration of social determinants of health (SDOH) and health equity practices within pharmacy and health care.

Payers, health systems, and health professionals will experience expanded accountability for performance in closing health disparity gaps in 2024.

Drug prices in the US increased 4.4% annually and median out-of-pocket (OOP) costs increased 9.6% annually from 2009 to 2018, but there was no direct link between these amounts for individual drugs.

The Center on Health Equity and Access delivers current updates, highlights breakthroughs in research, and ongoing endeavors committed to addressing healthcare inequalities and improving universal access to exceptional health care.

Promoting health equity isn’t only about consideration of underlying health risks; it’s also about using that data to inform population care as well as give clinicians and their teams more time with the patient in front of them.
What We’re Reading: ACA Sign-Up Surge; Hospitals Fight Climate Change; Secondary Cancers, CAR T Link
A record 21.3 million people signed up for health insurance this year using the Affordable Care Act (ACA) marketplaces; nearly 80% of health care providers think it is important for their hospital to minimize its environmental impact; the FDA noted a potential link between CAR-T products and the development of T-cell cancer.
CMS has announced new federal rules that require health insurers to streamline requests to cover treatments; nearly 50,000 veterans used the emergency suicide prevention program launched by the Department of Veteran Affairs in 2023; the FDA recently authorized the first artificial intelligence (AI)-powered medical device to help doctors detect the most common forms of skin cancer.

The findings demonstrate the critical need for immediate policy reforms to tackle structural racism and promote equitable pediatric care in the US for children regardless of race or ethnicity.
Families with workplace health insurance may have missed out on $125,000 in earnings over the past 3 decades due to rising premiums; so far, there have been about 600 drug price hikes in January; experts worry that minority and low-income people will not have easy access to zuranolone, the first FDA-approved postpartum depression pill.
Health insurance enrollment through the Affordable Care Act (ACA) insurance marketplace has broken a record for the third consecutive year; attention-deficit/hyperactivity disorder (ADHD) treatment prescriptions for adults surged during the COVID-19 pandemic, contributing to lingering shortages; paying high rent can shorten your lifespan.