Policy
Latest News
Latest Videos

Podcasts
CME Content
More News

ACOs serving patients with complex needs are on the rise, but policy changes are needed to support providers treating special populations.

The number of Black, Hispanic, and Latino students admitted into medical schools fell as rates increased for White and Asian students.

Kelley L. Julian, PharmD, BCOP, discusses optimizing myeloma care, addressing barriers in access to intravenous immunoglobulin and innovative therapies at Huntsman Cancer Institute.

AstraZeneca has struck a deal with the Trump administration to sell lower-priced drugs via TrumpRx, following a similar agreement with Pfizer.

Vivek Subbiah, MD, says artificial intelligence (AI) should assist clinicians in precision oncology, not replace human decision-making.

Explore the implications of the Most Favored Nation Order on US drug pricing reform and its potential impact on patient access and innovation.

UC Davis Health enhances patient care through a shared services center, ensuring continuity of care and optimizing pharmacy growth strategies.

The positive aspects of the executive order focused on homeless individuals, have been overshadowed by aspects not viewed as positively.
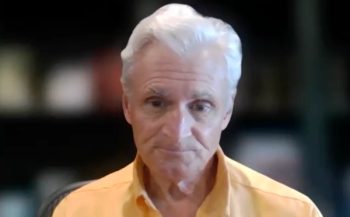
Robert Andrews, CEO of the Health Transformation Alliance, addresses Medicaid rebates, cost-shifting concerns, and value-based pricing trends.
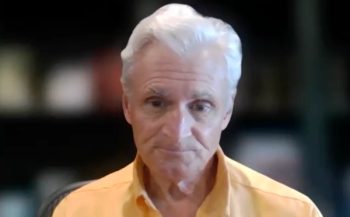
Robert Andrews, CEO of the Health Transformation Alliance, discusses the implications of the new TrumpRx platform on drug pricing policy.

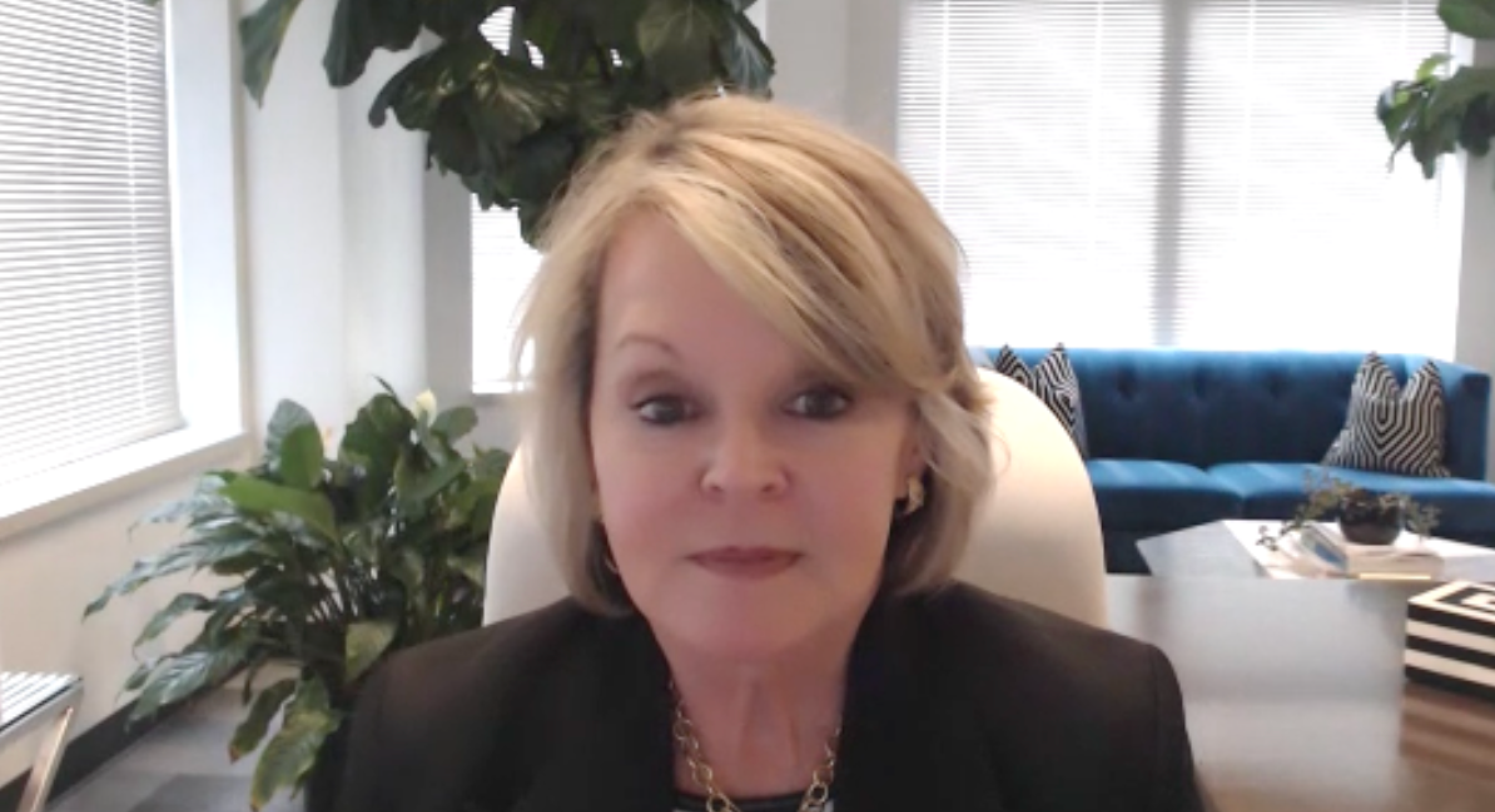
Laxmi Patel of Savista discusses how the Budget Reconciliation Act could widen Medicaid coverage gaps and strain hospitals across states.

Public health must address emotional and structural inequities, emphasizes Perry N. Halkitis, PhD, MS, MPH, dean of the Rutgers School of Public Health.

Today, Amgen announced the launch of AmgenNow, a direct-to-patient program offering evolocumab (Repatha) at nearly 60% below the current US list price.
The European Respiratory Society (ERS) Congress fosters collaboration among global experts, advancing respiratory health and promoting equality in medicine.

To mark the 30th anniversary of The American Journal of Managed Care, each issue in 2025 includes a special feature: reflections from a thought leader on what has changed—and what has not—over the past 3 decades and what’s next for managed care. The October issue features a conversation with Ge Bai, PhD, CPA, professor of accounting at Johns Hopkins Carey Business School and professor of health policy and management at Johns Hopkins Bloomberg School of Public Health in Baltimore, Maryland.

The US government shutdown could lead to telehealth, ambulance payment, and insurance cost disruptions.

The Trump administration advances the Most Favored Nation order by partnering with Pfizer, which came to the table voluntarily and has been granted a reprieve from upcoming drug tariffs.

Experts at the ERS Congress 2025 highlighted threats to scientific integrity from misinformation, political interference, and predatory publishing in health research.

Laxmi Patel explains how providers can meet potential new Medicaid documentation requirements without harming patient access.

A RAND report shows Medicare’s 3-year insulin savings model cut costs, improved access for beneficiaries, and offers lessons for future drug pricing reforms.

Oncology stakeholders are navigating new policies as the landscape quickly evolves, according to Ryan Haumschild, PharmD, MS, MBA, CPEL.

Explore cutting-edge discussions on patient-centered oncology, value-based care, AI innovations, and survivorship strategies Thursday and Friday at PCOC 2025 in Nashville.

Proposed Medicaid cuts threaten children's health coverage, exacerbating existing gaps and impacting access to care for vulnerable populations.

The Trump administration highlighted a potential autism risk from prenatal acetaminophen use, but studies demonstrate conflicting evidence.

Laxmi Patel outlines how Medicaid reforms could raise bad debt, urging providers to strengthen financial counseling, assistance, and price transparency.