Clinical
Latest News
Latest Videos

CME Content
More News

Panelists discuss how real-world evidence plays a crucial role in shaping both clinical decision-making and coverage policies for HER2-directed therapies in NSCLC, while exploring collaborative strategies between payers, providers, and manufacturers to balance equitable access with cost management.

There are a few unmet needs in schizophrenia that can make a big difference in the prognosis and quality of life of patients.

New research helps explain why a subset of patients with relapsing/remitting multiple sclerosis (MS) experience long-term heart rate slowing after taking fingolimod.

These authors investigated the potential influence of gut microbiota on ankylosing spondylitis pathophysiology.
New phase 3b data reveal significant skin clearance in historically underserved patients with moderate plaque psoriasis, offering hope for improved treatment outcomes.
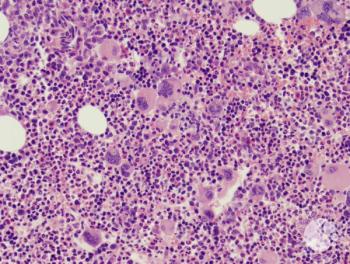
Experts are asking whether the study and treatment of myeloproliferative neoplasms (MPNs) is ready for a new era with new end points, with data that show how survival benefits are biologically linked to changes in the spleen, reduction in fibrosis, or other responses.

In part 2 of our interview with Surbhi Sidana, MD, MBBS, American Society of Hematology and Stanford University, she delves into one of the hottest topics in the hematologic malignancy space today: minimal residual disease (MRD) status.

There can be a delay in diagnosis of myeloproliferative neoplasms as the symptoms of the diseases can be variable and common, such as fatigue, migraines, and difficulty concentrating, explained Ruben Mesa, MD, of Atrium Health.

Moderate prediagnosis adherence to dietary guidelines was associated with improved survival rates among Black women with high-grade serous ovarian cancer, the most common and lethal type of ovarian cancer.

Toby Maher, MD, PhD, discusses how common signs and symptoms of idiopathic pulmonary fibrosis (IPF) at diagnosis can indicate disease progression, while also identifying key risk factors associated with IPF and emphasizing the importance of modifying certain lifestyle factors to help prevent the disease.

Toby Maher, MD, PhD, discusses how comorbidities complicate the diagnosis and management of idiopathic pulmonary fibrosis (IPF) and influence treatment decisions, highlighting the need for a comprehensive approach in patient care.

Toby Maher, MD, PhD, discusses how idiopathic pulmonary fibrosis (IPF) is diagnosed through specific imaging and tests, with an average diagnosis time that can delay effective treatment, emphasizing that early diagnosis is crucial for reducing disease severity and expanding available treatment options.

Interstitial lung abnormalities (ILAs) in patients with chronic obstructive pulmonary disease (COPD) are linked to lower lung adenocarcinoma rates but higher rates of other cancers and heart failure.
A new subgroup analysis of patients with muscle-specific tyrosine kinase (MuSK) autoantibody-positive (Ab+) myasthenia gravis (MG) shows rozanolixizumab (Rystiggo) contributes to meaningful symptom improvement.

Panelists discuss how unmet needs in type 2 inflammatory diseases require further research, including developing more personalized treatment approaches, identifying novel biomarkers for better disease phenotyping, improving long-term disease control strategies, and addressing the psychosocial impacts of chronic inflammatory conditions to enhance patients’ overall quality of life and outcomes.

Patients were found to have similar completion and yield rates for the fecal immunochemical test (FIT) at both 45 years and 50 years, making screening for colorectal cancer (CRC) effective in younger patients.

By 2021, neoadjuvant chemotherapy followed by interval cytoreductive surgery became the most common initial treatment for patients with advanced epithelial ovarian cancer, overtaking primary cytoreductive surgery.

In addition to Cobenfy being approved for schizophrenia, there are other drugs with novel mechanisms being studied that may mean combination therapies or, at least, more options for patients in the future.

Posters presented at the CHEST 2024 annual meeting revealed that delays in diagnosing fibrotic interstitial lung disease (ILD) can negatively impact overall survival, while supplemental oxygen therapy may exacerbate clinical burdens through increased rates of acute exacerbations and hospitalizations.

Examining care transitions in hospitalized patients revealed lower diagnostic error rates compared with traditional methods, highlighting the effectiveness of this approach in identifying diagnostic challenges.

While treatment options are evolving cancer care and extending lifespans, there is still a lack of biomarkers in certain cancers that can help direct treatment or provide early detection.

The panel of experts concludes by exploring the implementation of cardiometabolic risk management learnings and the utilization of telehealth in clinical practice.

Panelists discuss how payer perspectives and access challenges impact the utilization of HER2-directed therapies in NSCLC, examining barriers to treatment initiation and persistence, aligning provider and payer priorities in outcome assessment, the role of real-world evidence in decision-making and policy formation, and strategies for collaborative efforts between stakeholders to balance equitable access with cost management.

Experts examine strategies for coordinating initiatives to enhance cardiometabolic risk management care, focusing on incentivizing providers to deliver high-quality care to patients with cardiometabolic conditions.

A panel of experts explores the objectives and design of the COORDINATE-Diabetes trial, discussing its potential impact on the treatment paradigm for diabetes management.