
Oncology
Latest News
Latest Videos

More News

Daily image-guided radiotherapy, when compared to weekly control, decreases the risk of recurrence and rectal toxicity, but is associated with an increased risk of second cancer, according to study results presented at the 2018 Genitourinary Cancers Symposium.

Robotic procedures have really exploded in prostate cancer, said Christopher Kane, MD, professor of urology, University of California, San Diego. Robotic radical prostatectomy is now the most common way a radical prostatectomy is done in the United States.

Black patients with prostate cancer are underrepresented in clinical trials due to eligibility requirements that exclude patients with benign ethnic neutropenia, according to a new study published in JAMA Oncology.

During a session at the 2018 Genitourinary Cancers Symposium, Peter Black, MD, professor, department of urologic sciences, University of British Columbia, discussed using molecular subtypes, the Coxen model, and gene mutations to select patients and therapies for neoadjuvant chemotherapy.

During a session at the 2018 Genitourinay Cancers Symposium, Abhishek Solanki, MD, MS, assistant professor, radiation oncology, Loyola University of Chicago discussed the role of immunotherapy in patients undergoing radiation therapy for bladder cancer.

With new guidelines on how to treat and manage muscle-invasive bladder cancer, Jeffrey Holzbeierlein, MD, FACS, professor of urology, director of urologic oncology, interim chair of the department of urology, University of Kansas Health System, provided insight into how the guidelines have changed the management of the disease at the 2018 Genitourinary Cancers Symposium.

This week, the top managed care stories included Indiana being approved as the second state to implement work requirements in Medicaid; research found 5-year survival rates for cancer are increasing; coverage from the American Society of Clinical Oncology's 2018 Genitourinary Symposium.

During a session at the 2018 Genitourinary Cancers Symposium, 2 doctors debate whether there is existing evidence for local treatment for patients newly diagnosed with metastatic disease.

For the first time, molecular therapies, such as radium-223, provide a survival-prolonging agent for men with advanced prostate cancer affecting the bone, explained Joe O'Sullivan, MD, FRCR, clinical professor, School of Medicine, Dentistry and Biomedical Sciences, Queen's University Belfast.

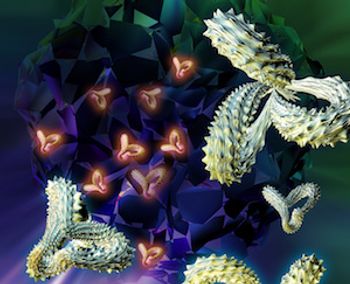
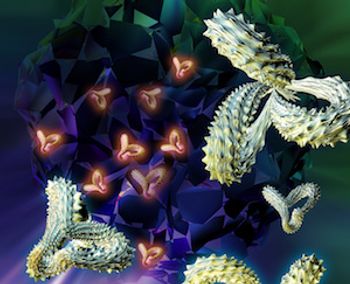
Osteomimicry may contribute to the uptake of radium-223 within bone metastases and may subsequently enhance the therapeutic benefit of radium-223, according to an abstract presented by Andrew Armstrong, MD, associate professor of medicine, Duke University School of Medicine, at the 2018 Genitourinary Cancers Symposium.

Apalutamide significantly improved median metastasis-free survival by 2 years in men with nonmetastatic castrate-resistant prostate cancer (nmCRPC), according to study results presented by Eric Jay Small, MD, MD, FASCO, chief of the division of hematology and oncology in the department of medicine at the University of California, San Francisco (UCSF), deputy director of the UCSF Helen Diller Family Comprehensive Cancer Center, and professor in residence in the Department of Medicine and Department of Urology, at the 2018 Genitourinary Cancers Symposium.
A long-term follow-up analyzing the toxic effects and results from a phase 1 clinical trial of adult patients with relapsed B-cell acute lymphoblastic leukemia (ALL) who were treated with CD19-specific chimeric antigen receptor (CAR) T cells found patients with low disease burden had a longer medial overall survival and a lower incidence of toxicity.
Patients with metastatic urothelial cancer treated with atezolizumab monotherapy demonstrated tolerability for the drug and general ability to manage adverse effects, according to a study published in JAMA Oncology.

While an increasing number of immunotherapies are reaching market and becoming available, cancer centers feel unprepared to prescribe these treatments and handle adverse events and side effects, according to findings from a new survey from the Association of Community Cancer Centers.

Before undertaking something like implementing the Oncology Care Model, practices should understand the scope of the project and the overall importance it can have for patient care, said Terrill Jordan, CEO of Regional Cancer Care Associates.

Cancer Mortality Statistics and Disparities in the US: Dr Patricia Salber Interviews Dr Otis Brawley
There has been some good news regarding cancer: a decline in the death rate and in new cancer diagnoses for men. However, the latest findings also highlight what still needs to be worked on, according to Otis W. Brawley, MD, MACP, FASCO, FACE, chief medical and scientific officer for the American Cancer Society.

When you have constant evolving contract, there are changes, and so some of the feedback I’m getting is that sometimes it’s hard to keep up with the changes, said Peter Aran, MD, medical director of Population Health Management at Blue Cross Blue Shield of Oklahoma.

There are a number of treatment choices available to treat patients with breast cancer and diagnostic tests can assist in the decision making, according to Adam M. Brufsky, MD, PhD, co-director of the Comprehensive Breast Cancer Center at University of Pittsburgh.

CONCORD-3 includes the records of 37.5 million patients diagnosed with cancer from 2000 to 2014, 322 population-based cancer registries in 71 countries and territories, and data on patients' vital status at least 5 years following diagnosis.

Every week, The American Journal of Managed Care® recaps the top managed care news of the week, and you can now listen to it on our podcast, Managed Care Cast.

This week, the top managed care news included President Donald Trump vowing to lower drug prices during his State of the Union address; 3 corporate giants joined forces on healthcare; and CAR T-cell therapy was named the cancer advance of the year.

Coverage of our peer-reviewed research and news reporting in the healthcare and mainstream press.

Researchers at the 59th Annual Meeting and Exposition of the American Society of Hematology in Atlanta, Georgia presented studies investigating the quality of life associated with various oncologic diseases.

New research on breast cancer biopsies and counseling after treatment will allow surgeons to have more meaningful conversations with their patients, according to a study published in JAMA Surgery.

Various presenters at the 59th Annual Meeting of the American Society of Hematology in Atlanta, Georgia discussed the cost of care involved in several different cancer treatments.
















